
Facebook whistleblower hearing: Frances Haugen calls for more regulation of tech giant – live updatesActors open up about getting naked on camera
Object Of The Exercise – December 2nd 2021


Carrie Johnson has revealed she was “moved to tears” when hearing from the victim of a hate crime at a Pride reception in Downing Street earlier this year.
The prime minister’s wife – who is pregnant with the couple’s second child – addressed an LGBT+ Conservatives reception at the Tory conference in Manchester on Tuesday night, during which she described herself as an “ally”.
Mrs Johnson told the packed event, which was also attended by her sister-in-law Rachel Johnson, that her husband was “completely committed” to “protecting those gains” made in past years by the LGBT+ community and “extending them further”.

Image Copyright Appledene Photographics.
Roberta Jane Cook will eventually require sectioning for the mental hospital according the NHS , Thames Valley Police Secret Reports And GIC Contracted Psychiatrist Dr C R Ramsay – And Records Too Upsetting For Roberta To Be Allowed To See. All parties to her diagnosis in response to her complaints against the police, have concluded that she is a paranoid delusional schizophrenic who must not see relevant police and NHS Records About Her. This Is Life In Police State Britain- Roberta Jane Cook August 19th 2021
He said she talked too fast but told him nothing about herself. He concluded that she is antisocial and can’t get on with people. He said if she saw all the secret reports about her she would be very upset – he wrote all of this in his report and lied that she refused a second opinion. He said she needs a multi agency approach which includes being watched by the police , but she doesn’t need hospital and sectioning just yet.
In 2016 , she was promised Gender Reassignment Surgery if she changed her name , took anti androgens , oestrogen and lived as a woman for two years. The Gender Identity Clinic received a mental health warning from Dr Roger Dickson’s Norden House Surgery in Buckinghamshire. They responded accordingly.
In March 2018, over the required two year living as a woman period, the Gender Reassignment Surgery was made conditional on her taking anti psychotic drugs.
Roberta refused , pointing out the utter pointless of sex change if you didn’t know who or what you were, also not being able to think or do anything worthwhile , in short agreeing to become a non person. These drugs have various side effects , including motor control, bladder control, bowel movements, balance issues and memory loss. She was working as a truck driver at the time this ‘baragain’ was offered. Its basis being a most intriguing and disturbing back story..
The drugs were refused. The situation led to further issues with the police which the NHS had called in to help them in a ‘multi agency approach’ to her case.
The results of a blood test from last May were not made known to her until July, when Dr Kamble spontaneously wrote promising full disclosure of secret correspondence with the Gender Identity Clinic.
That offer has since been withdrawn. The blood test results showed very low oestrogen and testosterone levels. As punishment for not accepting the multi agency pressure to take anti psychotics, Roberta’s hormone prescription has been cancelled. A palliative has been prescribed to cope with resultant bone and joint issues. By faking the date of the blood tests as last July , the GIC and Norden House have made an excuse to delay a due September test until December. The proverbial mind boggles. .
She has also suffered depression from this cancellation. She now faces court for her responses to over 13 years of harassment, with jail and mental hospital threats because she would not accept anti psychotics and shut up The next four monthly blood test has been based on the late July issue of results , rather than May, so her health condition deteriorates rapidly..
Caption and image copyright Roberta Jane Cook
True Blue – August 18th 2021

Image Appledene Photographics.
Writer Of Wrongs – Whore’s Tale by Roberta Jane Cook- August 7th 2021

Image Copyright Appledene Photographics.

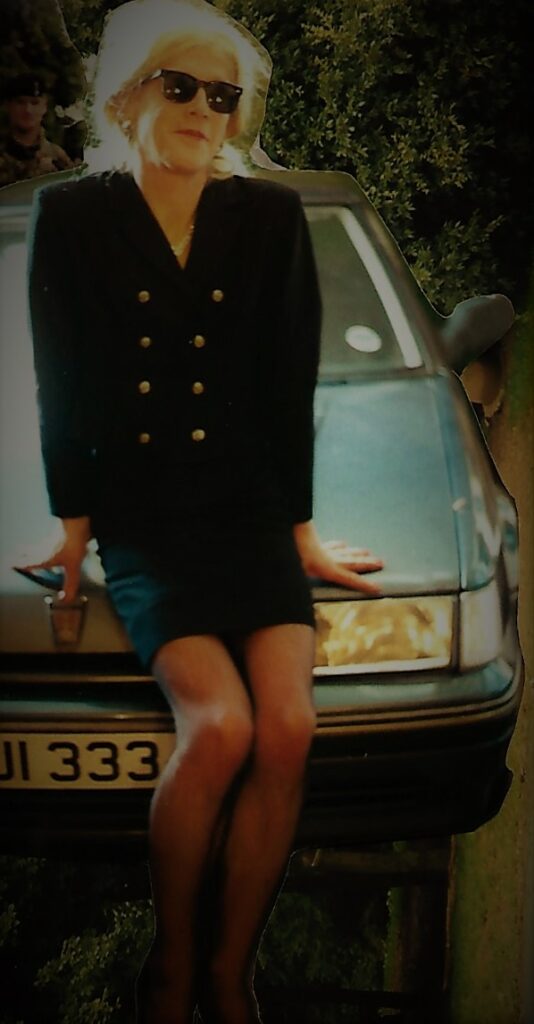
It is also important to note that I am wearing the same dress and jacket as , from the first picture and living as a woman, as part of the Gender Identity Clinic as gender treatment commitment , mandatory two years on hormones before surgery.
I mentioned my friendship with Lasio to only one person ,the owner of the dress. Being friendly with men is , I would have thought to be a reasonable thing for a girl to do. I am a very friendly and sociable with all nice people , though I might talk rather too much. Image Copyright Appledene Photographics. 2017.

Four years later, when I ended the relationship because of the dress owner’s attitude to my son, she told me sneeringly ;The police have been round here a lot. They told me you are transgender”. I don’t know if that is true , though it fits the Bill , if you will pardon the pun. I also know she told lies because she told me she did after telling me I was no good at lying because she was good at it.
I will write more about how , during my first visit to this woman’s home, I was the subject of night time surveillance by three Herts Police vehicles. It was late 2011. I will explain why I asked this friend to do a Claire’s law background check on me and what she said they had told her. Later , hopefully by this evening. The dress , remember is important to the story. So are the police. Roberta Jane Cook.
Image Copyright Appledene Photographics.
I have a restraining order which the police appear to believe is a gagging order. It derived from my response to knowledge that I had been given a malicious PNC Criminal Marker and ‘soft intelligence’ records by West Mercia Police on October 9th 2008, during my divorce . The police persist in official lies that they they investigated and appear to have forgotten their written warning as to what would happen if I persisted with my complaint and that there had been no investigation and never would be.They said that they were applying for an IPCC dispensation to dismiss it. It came to light when I applied for enhanced CRB Clearance to stay with a female musician friend in her flat at exclusive Woldingham School in Surrey in 2009.
When I inquired with the CRB , about the 71 day delay up to that date, I was told in writing that Thames Valley Police could not clear it until West Mercia Police disclosed their local soft intelligence against me. The month was May 2009. The situation urgent, I complained again and the clearance was miraculously approved. The existence of the PNC Criminal Marker was confirmed in writing by Chief Superintendent Mike Tighe of Thames Valley Police. He stated that he could not explain why it was created by West Mercia Police because the records were sealed. I have never lived in the West Mercia police area.
I spent well over 18 months trying to get to the truth. Eventually clearing me to stay in a flat an unlocked landing away from the 9th year girls dormitory was either an act of extreme negligence or secret admission that the records were malicious and motivated by police malice at a personal level.
Whatever, under the stress and not wishing to embarrass anyone at Woldingham with inevitable police conflict and publicity, I ended my relationship with the Woldingham House mistress and our work as song writers and performers of music. My son and I did , however, stay over at Woldingham many times. Here I attended mass , wined and dined at weekends. It is a Roman Catholic Boarding school.
Quite soon, in the wake of my devastating first court hearings, I was befriended by a woman who appeared to have read about me. That woman was the owner of the pretty jacket and dress that I am wearing in the top three pictures.
She invited me to visit soon after. I parked my car in a cul de sac near her house on a middle class estate in a town just north of London. She was sitting with me in the dark , in my car, about to say goodnight as I planned to head home. As we sat there , a convoy of Hertfordshire Police vehicles made three runs past us, turning around in a reversing area a little way behind us. As the Police Transit passed us the first time, I noticed the front passenger seated officer held a clip board and was staring in at me. I was being scrutinised. Remember the PNC Criminal Marker on my car.
Over a significant period of time, this surveillance became unbearable and I did not feel safe having a female relationship. Sometimes the surveillance cars were unmarked. One night, having returned with friends from a West End Theatre, we were outside bidding them good night. A small blue Ford pulled up , with a rotund officer asking us where number 24 was. His dashboard featured a large computer screen for sat nav and other intelligence sources, We were outside number 36. He appeared to be sniffing the air.
This was just part of my new normal life as a divorcee. It was intolerable and I am surprised that I am still alive. This was not any version of freedom.
So in 2014 , after a failed attempt to have my restraining order lifted , based on new evidence that I had been the victim of spurious stalking and violence allegations, I asked my female theatre friend to make a Claire’s Law disclosure application. I stayed in her bedroom when the officer arrived, I think from Welwyn Garden City. Some weeks later my friend said that they had disclosed nothing of concern. She quoted them as saying ‘Well you get on alright with him. Let sleeping dogs lie.’
After that I realised that the relationship was doomed. As I had done when my marriage was clearly not working out – something I realised within the first year because I was not compatible with my fiance’s family , especially her mother .
So I felt drawn toward making my longing for a female identity and to express it. Stupid people, especially self interested feminists confuse transgender with transvestitism. The latter are simply fetishists finding comfort and relief in proximity to the feminine garments, especially underwear. This is not the place to digress onto that subject , but I do know what I am talking about.
The relationship inevitably changed and was doomed. My friend became very aggressive toward myself and my son, insisting that I must choose between him or her. She caused many conflicts between us , leading me to venting at the police because I knew where this had come from. I decided that I should do what I should have done in the first place and come out as transsexual. then she would end the relationship without making me feel guilty. I wanted her to end it. I am a coward , you see. This is why I have done my best to avoid argument with the very powerful unaccountable police.
In the run up to my marriage, I was working as a progress chaser for a U.S defence contractor on Portsmouth Airport. One morning , my PA said to me ‘You don’t want to go through with it, do you?’ I said ‘No’. She said why do it then?’ I replied ‘Because I don’t want to upset her.?’ I felt I had a responsibility to go through with it. Ending it 31 years later , with two young adult sons – one in his final months at university and going on for legal training with ambitions to be a barrister- should not have been the nightmare that it became very quickly , but that s another story.
But it wasn’t easy breaking from my new friend. When I told her that I was transsexual, she replied :’You can have your sex change as long as you keep your penis.’ I replied ; ‘That is rather defeating the object of the exercise..’

By 2015, I had become used to her giving me pretty dresses to wear, while helping with perfume , make up and doing my hair. I was being treated as and dressed like her life sized doll. My escape plan had failed. So , that is how I came to be wearing the dress that I am wearing in the picture above. it is also how I came to have my house raided , property taken, spent 6.5 hours in a police cell following allegations that I was working for my son, as a ‘gay escort’ and his associates at my home which had been under surveillance as some kind of brothel. Once again, I ended up in Crown Court during the summer of 2018 as a result of this. I had apparently written to police calling myself a ‘gay’ escort. As point fact , we transsexual females do not call ourselves gay , though some of us might be lesbians. Whatever , that is not relevant to the term gender identity. Whatever , I had merely wished to be perceived and treated as female. Thus the police et al were committing a hate crime against me. They dragged me into Crown Court over it.

Image Copyright Photographics..
In 2016, following seven traumatising Crown Court hearings on charges where I was eventually found not guilty, I took leave from work and overdosed on tamazapam , so badly I woke up unconscious in Milton Keynes hospital due to police intervention. At ths point, I realised that I had to end my relationship with the friend who lived just north of London. I also realised that I needed to present myself at the local doctor’s surgery to discuss gender reassignment and appropriate eventual surgery to follow two years of living as a woman.
Fortunately my new GP was an understanding 30 something woman. I recall liking the dress that she was wearing. She listened carefully and patiently, promising a referral to the local adult mental health care unit with Dr C R Ramsay at Whiteleaf in Aylesbury. I had two consultations with him , one at his workplace and a home visit. His report was generous and supportive. Hence my referral to the London Tavistock Gender Identity Clinic.
I was their patient for over the two years necessary to be listed for Gender reassignment Surgery in March 2018. By this time matters had turned very sour. In 2017, I was made aware of significant correspondence from Norden House Surgery to Tavistock Clinic’s urologist Leighton Seal. He referred to five interesting letters – I saw one that originated from Reading Police Station in 2017

Image Copyright Appledene Photographics.
The implication of these letters was that I was a violent deranged alcoholic who could not be taken seriously as transsexual – and that I drank so much that my liver would not cope with the hormone treatment. I was sent to Stoke Mandeville Hospital High Wycombe – where there was a specialist scanning unit on Cressex Industrial Park – for countless test to prove a point, while all the time my seriously raised SHBG level was put down to heavy drinking – allegations originally made behind my back by my ex wife to our family GP in 2006.
Hormones and anti androgens were eventually agreed, but my GP surgery principal put up major resistance to a key anti androgen injection. these injections were crucial to balancing hormone levels prior to surgery. It is a delicate process because continue the process too long – as they did- and there is a withering of genital material for constructing a functioning vagina and facilitating sexual sensitivity – i.e orgasm.
In short one is in danger of being turned into a eunuch. So it crosses my mind that there was a constructive attempt to ridicule and undermine my gender reassignment for reasons it does not want to disclose. My card was being marked. Hence my new GP Dr Kamble going back on his written promise to disclose all correspondence, saying on record that there is too much for him to go through. To my request that he send all of it, he did not respond.
Image Copyright Appldene Photograaphics.
Following a road accident in February 2017, while driving a truck in the West Country on an icy foggy road, during the early hours, I took a break from truck driving to work on a novel about a murdered transsexual who had a death wish and attempt my memoirs. It came from a sense that society has serious underlying hostility to transsexuals and many commit suicide because of it – after long suffering in silence.
The accident and years of police induced stress had gotten the better of me. I feared for my powers of concentration so came off the road for everyone’s sake.. I was evasive when my theatre female friend who ridiculed my driving work as well as my son ,pressed for me to go south to live with her. . The relationship soured as a result and I ended it , effectively in March 2017. Matters came to a head when she said that the police had told her that I had lied to them about everything , including the suicide attempt for which they had called an ambulance in December 2016. I considered this an echo of her Claire’s Law response.
This was a red rag to me. So I tried to phone the police to challenge them. My friend obstructed me , so I ran outside to phone. She was not properly dressed so just stood shouting at me from her front door, to come back in. By this time I was connected. Only I had forgotten that I wasn’t in the Thames Valley area. Unfortunately I had already been connected to Hertfordshire Police and the operator heard my friend shouting , commanding me to comeback in. I told the police person that I had made a mistake and went back indoors.
Not long afterwards, the police, who had tracked my call, were knocking at the door and I was treated as a domestic abuse victim- apparently. However , it was insinuated that I ‘might’ be mentally ill. So I suspect, quite reasonably , that there was much more to the Claire’s law disclosure than my friend had told me.
Afterwards , came the first mention of the police being regular visitors to my friend’s house, and telling her that I was , in her word < TRANSGENDER. I don’t think she meant that I was the embodiment of transgendered people, but being half Greek seemed slightly dyslexic in English. This point is important as the story develops toward me being arrested in connection with the most unusual prostitution allegations ever. As an accomplished writer and researcher, I could not have made this account up – and wish I was just deluded. Then pills might help. as a kind of death…
I returned only once to see my friend after that, but was pursued when I confirmed our break up , by some very nasty abusive e mails and a phone call where she said aggressively, ‘I hope you and your son both go to prison for a very long time. That is what you deserve. I hope you die there.’

Well , contrary to all the poison spread about me. I am not an alcoholic , but I did need a few drinks after that. Significantly I didn’t drive trucks again until the following May, called to collect a truck , for my old employer, from Cardiff because the driver had run out of hours. I was driven down by taxi , the young Moslem driver knowing of my popularity with my pupils in Aylesbury, both of us knowing many Moslems from my era. We had a lot to talk about , including racism and Islam. He took a selfie with me in the truck stop. But when he drove off with the stranded Polish driver and I attempted to start the truck – after doing the legal check sheet of course- I discovered it had also broken down. I had to wait many hours for repairs.
I didn’t want to go straight back to my old job because I was still writing, so I went back on the agency. Pretty soon I was back on my usual long hours due to driver shortages. In October 2017, I was deployed to work delivering and fitting large domestic appliances, like expensive American fridge freezers, from a base near Aynho in North Oxfordshire It was a fun job, either going out with a driver’s mate or co driver ,depending on the size of the vehicle. Christmas was coming and I was very busy covering long distances and loving every minute of the long hours and endless roads. My dad left the army to be a truck driver and it was in my blood,
By ths time I was so engrossed that I had forgotten all about my lady friend from theatre land in her house just north of London.. A serious mistake, a woman scorned and all that.

Image Copyright Appledene Photographics…
My travels for ‘Swift Care’ between October 2017 and December 2018 were very interesting and a story in its own right. By February 2018, I was back working long shifts for my old employer and on a rest day. Because I always worked Saturdays, and shifts were legally limited to five days and six, my rest day was always on a Monday, On this particular Monday in February 2018 , there was a very loud signature banging on my front door. The house is up a lane with a large drive and field opposite. When I opened the door , I noticed police vehicles and a uniformed officer with a party of plain clothes officers behind him, including a female.
They demanded entry, the lead officer DC Bellamy, shouted ‘You are under arrest.’ Dismayed, I asked what for ?

Roberta did not discover the records until released by West Midlands CPS in 2012 , attempting to have a related restraining order overturned so that they could be challenged in court.
She has never been officially confronted with any violence allegations and was hundreds of miles from the site where she was allegedly stalking certain parties over the weekend of October 4th/5th 2008 , She was, with her son, in Lancashire and mourning the loss of her mother at the time..
Image Copyright Appledene Photographics.
I asked what I was being arrested for , while the other officers swarmed into and around the house. Breach of restraining order. You sent letters and images of a personal and private nature to your ex wife, her brother and their employers.
I was speechless as I was led away, a hand on my head as I was pushed down and into the back of a police car , then taken to the police station. Here I went through the usual routine, confirming my name etc, property put into plastic bag , finger printing and DNA taken al again, shoes and socks removed outside the cell door, where I was left to wonder for the next 6.5 cold smelly lonely frightening hours before hearing marching footsteps echoing down the grim stark corridor. The heavy lock clanked open and I was taken to the interview room There , I was left with a young African duty solicitor who immediately told me to plead guilty – on the basis of what police had told him. I said no and the two main officers, male and female entered the room. I was about to be presented with ‘evidence’ of something I could recall nothing about.
I was presented with a copy of the letters circulated to six people of significance, a picture of me, shown in the sequence above, laying on my Polish Chef friend’s bed wearing’ The Dress.’ The other picture, purporting to be of my wife, was of an attractive blonde middle aged lady in expensive lingerie and stockings. She was a total stranger but had been identified as my ex wife. The last picture puzzled me. But the first one was the vital clue. It had been taken and e mailed to me by my Polish friend who had taken it. Only one person had been given my permission and access details for e mails – my ex friend who had loaned me ‘The Dress.’
The second clue was the content and style of the letter. It was typed and unsigned. There was , however, a name. I cannot give the full name, but the name that should have been Lasio read as Lazar. The name had been lifted from the e mail address that came with the picture of me on this man’s bed, in ‘The Dress.’ As i said, my theatre dress owning former friend was rather dyslexic in English.
The letter contained, in dyslexic style, allegations that I was working from home as a ‘gay escort’ for my son and his associates. Clearly an attempt to criminalise me and my son to an ever eager police force , from a person who knew all about my police and court issues, along with ex in law details. This person was well equipped to fill in the gaps on google.
The most amazing bit was yet to come. It was alleged that either myself or son had sent the material following an argument – the police are aware, as was my theatre dress friend, that what has been done to us has caused serious stress and massive survival problems which the police do not wish to hear let alone address.
So to me questioning as to whether they had done any forensics on the material, such as finger prints, I was told ‘No’. The lead officer DC Bellamy went on to allege that the post mark indicated I posted them in Northampton on December 12th 2017. This large town is 25 miles from my home. I learned that my home had been under surveillance since the previous October. This was very odd. When I said that I had been working for Swift Care that day , and miles from Northampton, with tacho and time sheet records to prove it, he replied ‘It might have been a different day.’ when I said I had records covering any day, so pick one’ he didn’t answer. It is interesting that the person who appeared to be the prime target of the photos and letter , gave a no comment response.
Weeks passed and I demanded an update. I was called to a second interview where Bellamy briefed my female lawyer for one hour before calling me in for questioning, My lawyer told me I could not ask questions of the officer and encouraged me to plead guilty, making a joke of the damning malicious still unexplained PNC Criminal Marker. She said ‘For all I know, I might have one.’ This suggested to me that she had either been told by police that I am mad or has no idea what PNC markers are and why they are so serious.
A total of three months passed before my patience snapped. My crucial driving documents, mobile phones, debit card and computers had been confiscated as part of an alleged investigation. There was no point in making an official complaint to the IOPC because so many malicious actions have created an institutional barrier of prejudice against me. It appears that even employers were warned about me. No one listens, hence my 2016 suicide bid because even though I was found not guilty , police still refsused to explain anything about events dating back to October 2008.. So I made several phone inquiries but Bellamy never replied. I ended up leaving swearing on his voice mail. This led me back into Crown Court for harassment, having dumped my lawyer who kept telling me to take a caution. The female judge told me that she had listened to the recordings in the order made, not the order the police sent them. She said ‘You were doing what the Americans call venting.’ My son gave impressive evidence.
However, though once again ‘ not guilty’ one can only assume that police malice went into overdrive to prejudice my GP and the GIC , making a mockery of my transgendered status, rendering me even more vulnerable to allegations of mental illness , including paranoia and schizophrenia. Hence the peculiar behaviour of Dr Kirpal Sahota at the start of my last GIC appointment which should have led to my surgical transition being completed long ago.
The physical , psychological and social harm done has been overwhelming. Since officialdom still refuses to listen and investigate, I have once again returned to the internet in a cry for help and to make the unpleasant facts known – some of them at least, there are far more things that cannot be said with court action pending. Once again it has drawn me into court. Why ?My surgery was made contingent on strong drugs for the spurious contrived paranoid personality disorder so called diagnosis which would have made me into a zombie, making any expression of sexuality impossible.
Forcing me to take drugs is calling me a liar , with absolutely no evidence to back their judgement They don’t need it , with a very tame and heavily policed media to help cover up. That is how the establishment works in twenty first century Britain.
Roberta Jane Cook

Image Copyright Appledene Photographics..
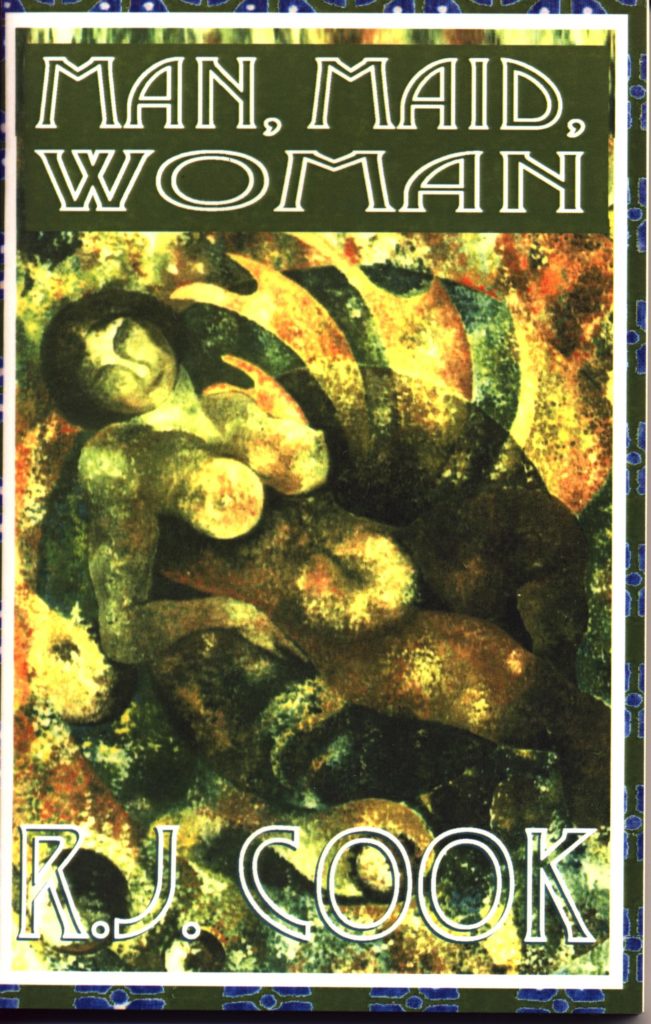
Editorial : Readers will note that R.J Cook has returned to using her legal rather than author name of Robert.
This is due to ongoing hate crime against her, mainly because of official attitudes.
She is Roberta Jane Cook, also signing as R.J. Cook – August 10th 2021.

‘You Are Not Working Class,’ Dr Kirpal Sahota of London’s Gender Identity Clinic , Adding ‘You Have A Secure Female Identity’ To Roberta Jane Cook August 7th 2021

The psychiatrist became party to a ‘multi agency approach’ which involved police monitoring and constant threat of being sectioned.
The psychiatrist came to his conclusions after three 45 minute home visits, following Roberta having carried out three 14 hour long distance truck driving shifts. The first one was unannouced , with two other NHS staff in case she had to be sectioned,. It is implied that Roberta simply fanatsises that she is a truck driver, after all, malicious police records were meant to stop her getting any work at all,.
Because she was sipping wine before going to bed for the next days’ work , it was used as further evidence to support her ex in laws recorded allegations that she is alcoholic.
These records include a PNC Criminal Marker dating from October 9th 2008, which the police still refuse to explain because their malpractice would incrimimate them at senior level . They simply go on lying to all cocerned parties, including the media and Gender Identity Clinic, that it ‘has all been invetigated.
Because she still refuses to admit that she is mad and delusional, her hormone treatmnet has been blocked causing serious health risks.More to come on how Thames Valley Police interferred to block her gender reassignment surgery
Sex Change Secrets – a comment related to the following two articles – by Roberta Jane Cook

This is Roberta Jane Cook in August 1988. She was not receiving hormone treatment but had lived with well below average testosterone – thus slowing progress toward puberty. The picture was taken by her ex wife;
Ironically I was first put into a girl’s dress as punishment. I was also forced to wear girls’ briefs. Dresses inevitably with all their bright colours ,frills and flounces influence behaviour. To avoid looking utterly stupid, I played the part and enjoyed it – all the more so because I was pre school and allowed to keep my blonde curls to shoulder length. Seeing my image in my parents’ wardrobe mirror, I couldn’t wait to get outside, sneakily taking a pair of my sister’s sandals to coordinate.
I just knew , better than my sister as I saw over time, what worked and what didn’t. My ex soldier lorry driver father died young due to misfortune. The only thing I know about his sex life apart from that it produced my sister and me, is a pamphlet I found while clearing out the old wardrobe when I returned home to live , in September 1979. The title was ‘How to achieve sexual ecstasy.’
My father was part of Britain’s ignominious Dunkirk retreat. He had seen a lot of death and dying. As a child visiting my terminally ill father for 9 months in 1962, I saw a ward full of condemned men, mostly worn out working class, prematurely aged like my father.Their death rattles became a familiar sound to me, until the Saturday in October 1962. Then it was my father’s turn to die.
Very little appealed to me about being a man. The vicious stupid comfortable people who embody feminism, with all its arrogance and contradictions, are most unappealing. As an aspiring woman, I do not wish entry to their herd or into the LGBTQI coral. I just want, at last, after 70 long difficult years, to be allowed to be me. I do not want the likes of ‘got lucky’ writer J.K Rowling telling me that I want sex change so as to lurk in ladies toilets to assault them.
I only know my own consciousness and wonder how the world could possibly persist without me being around to perceive it. Consciousness is still an enigma, and never more so when we apply the term to the very political world of sex change and female empowerment.
I have to say that the female masses, in my view,lack the style and elegance of the women I envied when I was growing up. I have to admit that we had much wealthier relatives where the women used to know how to dress, so as a 12 year old I started practising by wearing cast off , shoes, dresses and lingerie from my petite and posh cousin in London – where most of our relatives lived. They were sent for my sister who was too big to fit them , and wouldn’t have liked the style anyway. My sister was at the grammar school where her academic ego and pugnacious personality flourished.
I went to great lengths to conceal my genitals – there are ways- so that I felt I looked good. I really hated my penis, though my female self knew why girls liked them and didn’t like men in dresses – just not sexy from their point of view. I read a lot of classic literature as a teenager, including Virginia Woolf. She wrote that ‘the way we dress has a big influence on how people see and judge us and on how we see ourselves.
Little attention is paid to the masses of women who have no interest in traditional female style and clothing. They are encouraged to look like and outdo the boys. They scorn transsexuals – very different people to transvestites who are fetishists pure and simple, never wanting the penises gone which is the essence of what we transsexuals want. The best place for a penis in our view, is inside us by consent.
But feminists, religious bigots and others can’t accept this as normality. To them we belong in a freak show.But lesbians and girls in male drag are cool’. Nor can they accept that their increasingly masculine dress and behaviour pushes males toward alternative expressions of sexuality. Transgender isn’t an outcome of one common cause.However, some of us show subtle signs of femininity which scientists have linked to mother’s hormone levels during conception and pregnancy. Ths would explain why transsexuality is a cross cultural phenomenon.
So we come to where we are now.My ex mother in law told me with a sneer that ‘You’re sick and in need of help.’ Her daughter told me that she wasn’t going to tell the divorce court ‘about your dirty little secrets.’ LGBTQ is no answer to this nasty mentality. It is a cage from which they can watch the world from a safe distance.
Now for legal reasons, I cannot go into detail as to how and why the police intervened with my GP to warn the London Gender Identity Clinic that I am mentally ill and have been for years. By chance, I saw the correspondence from Reading police station.My GP was not supposed to show me , let alone draw my attention , then leave the room while I photographed it off his VDU. There are complex reasons for the police’s interesting and alarming attitude to me , but with a court case pending I cannot say more.
Suffice it to say, that in March 2018 , after living openly as a woman for 2 years, with all of the cost and attendant risks, I should have been lined up for gender reassignment surgery. But Thames Valley Police put the icing on the cake by arresting me because of anonymous material and photographs to significant parties. One was a picture of me that could only have come from an aggrieved dumped ex partner. The other was of a stranger dressed in lingerie , described in six typed unsigned barely literate letters, as my ex wife.
It was alleged that I had been working as a gay escort for my son and his associates. Because of their ‘he’s mental routine’ they alleged that I informed on myself to get him into trouble. They had no evidence and were unresponsive when I told them who the culprit was . They said they had been watching the house for 3 months but, presumably, failed to notice me going out to my truck driving shift every night at 01.00 in the morning.
The case petered out but I was taken t court for swearing on the lead officer’s voice mail. The judge exonerated me. There has been a lot more of this over the last 13 plus years.This is just a taster as to how the Gender Identity Clinic made my sex change surgery contingent on mind destroying anti psychotic drugs .
The police have worked very hard to persuaded my GP and the Gender Clinic that I am a sex mad violent lunatic. Now just as we approach a definitive Crown Court hearing, that same clinic has conveniently cancelled my hormone treatment after 5 years of brain and body altering effects – offering only the comfort of waiting to see more psychiatrists so that, as long as I accept being deluded, I might start the gender reassignment two year programme again.
Obviously quite ludicrous giving that I am approaching 71. This of course is about keeping our police and NHS free from criticism and damages claims.
You will read below just how serious being deprived of oestrogen will soon become for me. As always with public services, stone walling is their first line of defence. Breach that and you are in very serious danger.
I will offer this posting to the GIC for comment. They have , like the police, ignored all of my previous requests for information and are well protected by a plethora of new laws. Roberta Jane Cook
Post Script I have now heard that Dr Kamble of Norden House Surgery has cancelled my prescription for tamazapam, causing me further anxiety. .
I recorded a phone conversation with him two days ago when I asked him where the promised letters were. He wrote to tell me that he had been reading my messages and realised that I had not seen all f the correspondence about me, going back and forth between the Gender Identity Clinic and Norden House Surgery. That was over a month ago. When questioned as to where that correspondence was , he acted as if he had forgotten. When pressed he said he hadn’t the time to sort it out because there was so much.
So I said just copy it all and make sure you send the one you got from Reading Police Station telling you that I have been mentally ill for many years and the Gender Identity Clinic should be warned. I explained that his colleague , Dr Ramasamay had brought it up on his computer screen , drawn it to my attention before leaving the room , thus giving me time to copy it on to my phone. R.J.C
Sex Change Hormonal Treatments Alter Brain Chemistry – August 6th 2021
Reports new study in Biological Psychiatry
Philadelphia, PA, October 8, 2015
Hormonal treatments administered as part of the procedures for sex reassignment have well-known and well-documented effects on the secondary sexual characteristics of the adult body, shifting a recipient’s physical appearance to that of the opposite sex.
New research published in the current issue of Biological Psychiatry indicates that these hormonal treatments also alter brain chemistry.
Researchers at the Medical University of Vienna, led by senior authors Dr. Siegfried Kasper and Dr. Rupert Lanzenberger, show that administration of the male hormone testosterone in female-to-male transsexuals raises brain levels of SERT, the protein that transports the chemical messenger serotonin into nerve cells.
In contrast, male-to-female transsexuals who received a testosterone blocker and the female hormone estrogen showed decreased levels of this protein in the brain.
SERT plays an important role in the treatment of mood and anxiety disorders, as many common antidepressants, such as Prozac, block its activity by inhibiting serotonin reuptake. In addition, some genetics studies have suggested that higher levels of serotonin transporter may increase resilience to stress and reduce risk for stress and mood disorders.
Because women are twice as likely to be diagnosed with depression as men, these changes in the levels of SERT are consistent with the increased risk for mood and anxiety disorders in females relative to males.
Lanzenberger added, “These results may explain why testosterone improves symptoms in some forms of depression. Our study also increases our knowledge on the role of sex hormones in sex differences of mood disorders.”
Overall, these findings suggest that when people switch from female to male, their biology changes in a way that is consistent with a reduced risk for mood and anxiety disorders, whereas the reverse happens when males switch to females.
“This study is the first to show changes in brain chemistry associated with the hormonal treatments administered in the sex change process,” said Dr. John Krystal, Editor of Biological Psychiatry. “It provides new insight into the ways that the hormonal differences between men and women influence mood and the risk for mood disorders.”
The article is “High-Dose Testosterone Treatment Increases Serotonin Transporter Binding in Transgender People” by Georg S. Kranz, Wolfgang Wadsak, Ulrike Kaufmann, Markus Savli, Pia Baldinger, Gregor Gryglewski, Daniela Haeusler, Marie Spies, Markus Mitterhauser, Siegfried Kasper, and Rupert Lanzenberger (doi: 10.1016/j.biopsych.2014.09.010). The article appears in Biological Psychiatry, Volume 78, Issue 8 (October 15, 2015), published by Elsevier.
—
Notes for editors
Full text of the article is available to credentialed journalists upon request; contact Rhiannon Bugno at +1 214 648 0880 or Biol.Psych@utsouthwestern.edu. Journalists wishing to interview the authors may contact Dr. Rupert Lanzenberger at +43 (1) 40400 35760 or rupert.lanzenberger@meduniwien.ac.at.
The authors’ affiliations, and disclosures of financial and conflicts of interests are available in the article.
John H. Krystal, M.D., is Chairman of the Department of Psychiatry at the Yale University School of Medicine, Chief of Psychiatry at Yale-New Haven Hospital, and a research psychiatrist at the VA Connecticut Healthcare System. His disclosures of financial and conflicts of interests are available here.
About Biological Psychiatry
Biological Psychiatry is the official journal of the Society of Biological Psychiatry, whose purpose is to promote excellence in scientific research and education in fields that investigate the nature, causes, mechanisms and treatments of disorders of thought, emotion, or behavior. In accord with this mission, this peer-reviewed, rapid-publication, international journal publishes both basic and clinical contributions from all disciplines and research areas relevant to the pathophysiology and treatment of major psychiatric disorders.
The journal publishes novel results of original research which represent an important new lead or significant impact on the field, particularly those addressing genetic and environmental risk factors, neural circuitry and neurochemistry, and important new therapeutic approaches. Reviews and commentaries that focus on topics of current research and interest are also encouraged.
Biological Psychiatry is one of the most selective and highly cited journals in the field of psychiatric neuroscience. It is ranked 6th out of 140 Psychiatry titles and 10th out of 252 Neurosciences titles in the Journal Citations Reports published by Thomson Reuters. The 2014 Impact Factor score for Biological Psychiatry is 10.255.
About Elsevier
As a global leader in information and analytics, Elsevier helps researchers and healthcare professionals advance science and improve health outcomes for the benefit of society. We do this by facilitating insights and critical decision-making for customers across the global research and health ecosystems.
In everything we publish, we uphold the highest standards of quality and integrity. We bring that same rigor to our information analytics solutions for researchers, health professionals, institutions and funders.
Elsevier employs 8,100 people worldwide. We have supported the work of our research and health partners for more than 140 years. Growing from our roots in publishing, we offer knowledge and valuable analytics that help our users make breakthroughs and drive societal progress. Digital solutions such as ScienceDirect, Scopus, SciVal, ClinicalKey and Sherpath support strategic research management, R&D performance, clinical decision support, and health education. Researchers and healthcare professionals rely on our 2,500+ digitized journals, including The Lancet and Cell; our 40,000 eBook titles; and our iconic reference works, such as Gray’s Anatomy. With the Elsevier Foundation and our external Inclusion & Diversity Advisory Board, we work in partnership with diverse stakeholders to advance inclusion and diversity in science, research and healthcare in developing countries and around the world.
Elsevier is part of RELX, a global provider of information-based analytics and decision tools for professional and business customers. www.elsevier.com.
Media Contact
Rhiannon Bugno, Editorial Office
+1 214 648 0880
Biol.Psych@utsouthwestern.edu
The Role of Estrogen in Brain and Cognitive Aging
Jason K Russell 1 2, Carrie K Jones 1 2, Paul A Newhouse 3 4Affiliations expand
- PMID: 31364065
- PMCID: PMC6694379
- DOI: 10.1007/s13311-019-00766-9
Free PMC article
Abstract
There are 3 common physiological estrogens, of which estradiol (E2) is seen to decline rapidly over the menopausal transition. This decline in E2 has been associated with a number of changes in the brain, including cognitive changes, effects on sleep, and effects on mood. These effects have been demonstrated in both rodent and non-human preclinical models. Furthermore, E2 interactions have been indicated in a number of neuropsychiatric disorders, including Alzheimer’s disease, schizophrenia, and depression. In normal brain aging, there are a number of systems that undergo changes and a number of these show interactions with E2, particularly the cholinergic system, the dopaminergic system, and mitochondrial function. E2 treatment has been shown to ameliorate some of the behavioral and morphological changes seen in preclinical models of menopause; however, in clinical populations, the effects of E2 treatment on cognitive changes after menopause are mixed. The future use of sex hormone treatment will likely focus on personalized or precision medicine for the prevention or treatment of cognitive disturbances during aging, with a better understanding of who may benefit from such treatment.
Keywords: Estrogen; aging; cognition; critical period; estradiol; menopause.
Figures



Similar articles
- From the 90’s to now: A brief historical perspective on more than two decades of estrogen neuroprotection.Engler-Chiurazzi EB, Singh M, Simpkins JW.Brain Res. 2016 Feb 15;1633:96-100. doi: 10.1016/j.brainres.2015.12.044. Epub 2015 Dec 29.PMID: 26740397 Free PMC article.
- Reprint of: From the 90׳s to now: A brief historical perspective on more than two decades of estrogen neuroprotection.Engler-Chiurazzi EB, Singh M, Simpkins JW.Brain Res. 2016 Aug 15;1645:79-82. doi: 10.1016/j.brainres.2016.06.016. Epub 2016 Jun 16.PMID: 27317847 Free PMC article. Review.
- Long-term consequences of estrogens administered in midlife on female cognitive aging.Daniel JM, Witty CF, Rodgers SP.Horm Behav. 2015 Aug;74:77-85. doi: 10.1016/j.yhbeh.2015.04.012. Epub 2015 Apr 25.PMID: 25917862 Free PMC article. Review.
- Estrogen-cholinergic interactions: Implications for cognitive aging.Newhouse P, Dumas J.Horm Behav. 2015 Aug;74:173-85. doi: 10.1016/j.yhbeh.2015.06.022. Epub 2015 Jul 14.PMID: 26187712 Free PMC article. Review.
- Action of estrogens in the aging brain: dementia and cognitive aging.Henderson VW.Biochim Biophys Acta. 2010 Oct;1800(10):1077-83. doi: 10.1016/j.bbagen.2009.11.005. Epub 2009 Nov 12.PMID: 19913598 Review.
Cited by 5 articles
- Protective Effects of Estrogen on Cardiovascular Disease Mediated by Oxidative Stress.Xiang D, Liu Y, Zhou S, Zhou E, Wang Y.Oxid Med Cell Longev. 2021 Jun 28;2021:5523516. doi: 10.1155/2021/5523516. eCollection 2021.PMID: 34257804 Free PMC article. Review.
- Insomnia, Inattention and Fatigue Symptoms of Women with Premenstrual Dysphoric Disorder.Lin PC, Ko CH, Lin YJ, Yen JY.Int J Environ Res Public Health. 2021 Jun 8;18(12):6192. doi: 10.3390/ijerph18126192.PMID: 34201084 Free PMC article.
- Protective effects of Lycium barbarum polysaccharide on ovariectomy‑induced cognition reduction in aging mice.Zheng X, Wang J, Bi F, Li Y, Xiao J, Chai Z, Li Y, Miao Z, Wang Y.Int J Mol Med. 2021 Jul;48(1):121. doi: 10.3892/ijmm.2021.4954. Epub 2021 May 6.PMID: 33955518 Free PMC article.
- The Role of Intranasal Oxytocin on Social Cognition: An Integrative Human Lifespan Approach.Horta M, Pehlivanoglu D, Ebner NC.Curr Behav Neurosci Rep. 2020 Dec;7(4):175-192. doi: 10.1007/s40473-020-00214-5. Epub 2020 Sep 12.PMID: 33717829
- A systematic and methodological review of attentional biases in eating disorders: Food, body, and perfectionism.Ralph-Nearman C, Achee M, Lapidus R, Stewart JL, Filik R.Brain Behav. 2019 Dec;9(12):e01458. doi: 10.1002/brb3.1458. Epub 2019 Nov 7.PMID: 31696674 Free PMC article.
Actor Denies Homophobia – August 3rd 2021
‘I stand with the LGBTQ+ community’: Matt Damon denies using homophobic slur
The balance of power among Labour’s factions is shifting under Keir StarmerStormzy hires karaoke bar for his birthday
Matt Damon has reportedly denied using the homophobic “F-slur” in his personal life and says he stands with the LGBTQ+ community following a backlash to comments he made in a recent interview.
The Hollywood actor, who is currently starring in the film Stillwater, has faced criticism after saying the word was “commonly used” when he was younger and that when he repeated a “joke” made in his 2003 film Stuck On You in front of his daughter, she wrote about “how that word is dangerous”.
After coming under fire on social media, Damon released a statement clarifying his comments to The Hollywood Reporter and Variety in the US, saying he does not use “slurs of any kind” and the conversation he was referring to “was not a personal awakening” but rather a discussion about how times have changed.
“During a recent interview, I recalled a discussion I had with my daughter where I attempted to contextualise for her the progress that has been made – though by no means completed – since I was growing up in Boston and, as a child, heard the word ‘f*g’ used on the street before I knew what it even referred to,” he said.
“I explained that that word was used constantly and casually and was even a line of dialogue in a movie of mine as recently as 2003; she in turn expressed incredulity that there could ever have been a time where that word was used unthinkingly.”
Damon said that to his “admiration and pride”, his daughter was “extremely articulate about the extent to which that word would have been painful to someone in the LGBTQ+ community regardless of how culturally normalised it was”.
The star said he “not only agreed with her but [was] thrilled at her passion, values and desire for social justice”.
He continued: “I have never called anyone ‘f****t’ in my personal life and this conversation with my daughter was not a personal awakening. I do not use slurs of any kind.
Comment If society continues like this we will have no brilliant actors like Damon, or mainstream writing worthy of attention. History is already being censored and rewritten by the likes of Woke and BLM. I see dangers with LGBTQI though understand why it had to exist. However, it is going the same way as feminism, especially TERFS as people cluster together either to attack or defensively. Multi culture separates people and is a con because all that is acceptable is defined by the ruling elite’s culture.
People will never find freedom this way and religious bigots will not accept LGBTQI because their attention is on God and success toward a better life. It is fundamental for them. That is why the likes of Rowling should shut up about transgender and her hate crimes be dealt with.
Feminists have the same fundamentalist adversorial tendencies as the religious bigots. For women like Rowling, their female parts are their status symbols, records of oppression and claim to power. They have politicised sex for their own glory – and made it a misery for many of us , especially those of us who are creative. Sadly , Rowling’s peculiar Hogwarts fantasy writing is what passes for good writing these days.

Roberta Jane Cook – aka Eleanour Cook, legal name change will follow as soon as possible , but the name Eleanour will replace Roberta in all further pience or comments of this kind..
“Because You Are A Woman”, Roberta recalls interesting moments from long ago and far away-August 1st 2021

He was driving me to a posh restaurant for lunch. Then , he said "You told me that you were bisexual in your letter, how would you know that if you've never even had sex?" I occupied myself by staring at the tips of my high heeled shoes. "I don't really, I suppose. I'm mostly attracted to men. Attractive men, like you." I smiled and risked a glance over at him. We were stopped at a red light and he was looking right at me. "Good lord, so you can be a flirt!" The light changed and he put the car in gear. I giggled, feeling like a fool. "I'm sorry." "Don't be, you're cute when you smile." "I did mean that," I said, feeling sheepish. "I know. What about other women?" "I am sometimes attracted to some women. It's different, though." "Different how?" "I don't know," I said, I really didn't know how to explain it. "I guess I always feel jealous of them." He nodded. "Makes sense." "Because I'm a transsexual?" He laughed. "No silly girl, because you're a woman!"
Prostate Pro (prostatepronow.com)
You have to be careful what you say nowadays. How about this? Referring to women as adult human females is apparently transphobic: https://www.spiked-online.com/2021/06/21/i-wont-let-these-arseholes-make-my-life-miserable/ F.S
Wally Stott composer – Bing images
- Wally Stott music, videos, stats, and photos | Last.fmhttps://www.last.fm/music/Wally+Stott14/01/2009 · Angela Morley (born 10 March 1924 – 14 January 2009) was an English composer and conductor. Morley was born transgender. born in Leeds, Yorkshire in 1924. Her birth name was Wally Stott. Morley played saxophone in a number of dance bands, and in 1944 became a member of Geraldo’s band. She attributed her entry into composing and arranging …
Wally Stott | Biography & History | AllMusic
https://www.allmusic.com/artist/wally-stott-mn0000361609
This British arranger, composer, conductor, and orchestra leader was nothing if not a class act. He designed musical backgrounds for vocalists who were simply dripping with personality, including the wonderful German vocalist and actress Marlene Dietrich and the brassy Dusty Springfield. Stott was also a mainstay of the British Broadcasting Corporation, leading in the early ’50s to a new …
J.K Rambling gets to the bottom of the transsexual issue.

Conversing with a Transsexual :
“Transvestites and transsexuals are very different creatures.” I said. “Obviously! So why don’t you explain to me what the difference is. Why is it that he always looks like a guy in drag and you don’t?” “But I do… ” I started to say. He held up his hand, interrupting me. “Explain the difference between a transvestite and a transsexual.” “I’ll try, it’s really kinda complicated. A transvestite is usually a man who gets a kick, usually a sexual thrill, out of dressing as a woman. A transsexual is someone of either gender who’s brain and body are out of synch.” “Out of synch?” “Well, in my case my brain is female but my body is male. To put it another way, gender is what’s between your ears, and sex is what’s between your legs. My gender is female, but my sex is male. This is not a good thing.” “In what way?” “It’s very destructive. For most people gender and sex are the same, so they never give it a second thought. But for me the two are at opposite extremes, forever in conflict.” “So how do you resolve the conflict?” “That’s were it gets complicated. I can’t change me, who I am inside, so I have to change who I am on the outside.” “And how do you do that?” I sighed, just thinking about it could be a little depressing. “Through a long, arduous, sometimes painful, and more than a little expensive process. First you go to an electrologist who starts the process of permanently removing facial and body hair. Then you see a shrink who evaluates you to determine if you can go further. If your shrink agrees then they will give you a referral to an endocrinologist who will do an evaluation and hopefully start you on hormonal therapy. The hormones, in my case estrogens, will change the body, feminizing it. That causes breast growth, fat redistribution, emotional changes, and a whole host of lesser changes. After that you’re supposed to live at least a year, and usually more than that, as your new gender. Then you can, if you wish to, go for sexual reassignment surgery. That’s were they will remove your penis and use parts of it to construct a vagina using plastic surgery. If everything goes well, in the end no one will ever have to know that you were ever anything other than a normal female in every way.” “Sounds like a hell of a lot of work.” “It is. In a way it’s like dying and being reborn whole. It’s the only way I can every be whole.” “So how far along are you in all of this?” “I’ve been seeing an electrologist for two years, and I’ve just recently started seeing a psychologist.” “An electrologist is the one who removes hair?” “Yes, removes it permanently.” “How?” “By sticking a tiny little needle underneath the skin where each hair grows,” I made a little motion like that was what I was doing, “and then zapping the follicle with microwaves or high voltage. If they do it right that kills the follicle and hair won’t ever grow there again.” “Ouch!” I laughed. “Bigtime, and you pay dearly for the privilege.” “So that’s why you don’t have a beard or anything?” I nodded. “I used to have some facial hair, never all that much, but it’s pretty much all gone now. We’re working on other areas now.” “And what about the shrink?” “I’ve only seen her a couple of times, but we get along pretty well.” Better than I had expected, actually. “What are you going to tell her about tonight?” “Not a thing. Don’t get me wrong, but I don’t tell her anything remotely resembling the truth, I tell her what she wants to hear.” “I don’t understand, why not tell her the truth?” “All I want from her is a referral to an endocrinologist. To get that I have to convince her that I am what I say I am, a transsexual. She has certain ideas about what a transsexual is or should be, so I’m going to do everything I can to fit into that mold. Look, it’s a screwy system, but that’s how the game is played. I don’t like it, but I really don’t have much choice.”
“Why don’t you live as a woman now?” “I’m not ready, not yet. No one is going to be willing to accept me as a woman now.” “That’s not true.” “It is true.” I hated contradicting him, but felt I had to. “Maybe after I’ve started hormonal therapy, but not now.” “That’s bullshit. You’re problem is that you’ve got no self confidence whatsoever, no self image. In fact I even doubt that you’ve got the foggiest idea what you look like and how other people perceive you.” That much was true, and something I forever wondered about. Something seemed to dawn on him. “Carol, what have your lovers thought of you? That certainly must have told you something. And by the way, do you mostly sleep with men or women? You said in your letter that you were bisexual.” My cheeks were turning red again. “I’ve never had any lovers.” “You’re kidding, right?” I’m sure my cheeks were burning brightly by now. “No,” I said, shaking my head and suppressing the urge to bite my lip. “How old are you?” He should know that, I told him my age in the letter. “Twenty-three.” “My god,” he said, laughing, “I’m sitting here with the worlds oldest virgin!” I was less than amused. “I’ve avoided sexual entanglements.” “Why?” “Because it would complicate things to much. I mean how am I going to have a normal sexual relationship? My situation, not to mention my body, kinda complicates things, you know? The most important thing to me is to be viewed and treated as a woman, and it never seemed much likely that I was going to be viewed as anything but a bit of a freak, at least until after hormonal therapy and surgery. I’d always planned on waiting until after surgery before trying to start a serious relationship.”
“Once I start hormonal therapy things will be set in motion that can’t be stopped, I’ll have to ‘die’. You don’t think that I can still keep the same job, the same apartment, the same friends once I’m a woman? I’ll never be a woman to them, only a freak. I don’t want that. Once I start down that road, I have to give everything up and start again anyway.”

J.K. Rowling Writes about Her Reasons for Speaking out on Sex and Gender Issues
July 27th 2021
Warning: This piece contains inappropriate language for children.
This isn’t an easy piece to write, for reasons that will shortly become clear, but I know it’s time to explain myself on an issue surrounded by toxicity. I write this without any desire to add to that toxicity.
For people who don’t know: last December I tweeted my support for Maya Forstater, a tax specialist who’d lost her job for what were deemed ‘transphobic’ tweets. She took her case to an employment tribunal, asking the judge to rule on whether a philosophical belief that sex is determined by biology is protected in law. Judge Tayler ruled that it wasn’t.
My interest in trans issues pre-dated Maya’s case by almost two years, during which I followed the debate around the concept of gender identity closely. I’ve met trans people, and read sundry books, blogs and articles by trans people, gender specialists, intersex people, psychologists, safeguarding experts, social workers and doctors, and followed the discourse online and in traditional media. On one level, my interest in this issue has been professional, because I’m writing a crime series, set in the present day, and my fictional female detective is of an age to be interested in, and affected by, these issues herself, but on another, it’s intensely personal, as I’m about to explain.
All the time I’ve been researching and learning, accusations and threats from trans activists have been bubbling in my Twitter timeline. This was initially triggered by a ‘like’. When I started taking an interest in gender identity and transgender matters, I began screenshotting comments that interested me, as a way of reminding myself what I might want to research later. On one occasion, I absent-mindedly ‘liked’ instead of screenshotting. That single ‘like’ was deemed evidence of wrongthink, and a persistent low level of harassment began.
Months later, I compounded my accidental ‘like’ crime by following Magdalen Berns on Twitter. Magdalen was an immensely brave young feminist and lesbian who was dying of an aggressive brain tumour. I followed her because I wanted to contact her directly, which I succeeded in doing. However, as Magdalen was a great believer in the importance of biological sex, and didn’t believe lesbians should be called bigots for not dating trans women with penises, dots were joined in the heads of twitter trans activists, and the level of social media abuse increased.
I mention all this only to explain that I knew perfectly well what was going to happen when I supported Maya. I must have been on my fourth or fifth cancellation by then. I expected the threats of violence, to be told I was literally killing trans people with my hate, to be called cunt and bitch and, of course, for my books to be burned, although one particularly abusive man told me he’d composted them.
What I didn’t expect in the aftermath of my cancellation was the avalanche of emails and letters that came showering down upon me, the overwhelming majority of which were positive, grateful and supportive. They came from a cross-section of kind, empathetic and intelligent people, some of them working in fields dealing with gender dysphoria and trans people, who’re all deeply concerned about the way a socio-political concept is influencing politics, medical practice and safeguarding. They’re worried about the dangers to young people, gay people and about the erosion of women’s and girl’s rights. Above all, they’re worried about a climate of fear that serves nobody – least of all trans youth – well.
It is influencing politics, medical practice and safeguarding. They’re worried about the dangers to young people, gay people and about the erosion of women’s and girl’s rights. Above all, they’re worried about a climate of fear that serves nobody – least of all trans youth – well.
I’d stepped back from Twitter for many months both before and after tweeting support for Maya, because I knew it was doing nothing good for my mental health. I only returned because I wanted to share a free children’s book during the pandemic. Immediately, activists who clearly believe themselves to be good, kind and progressive people swarmed back into my timeline, assuming a right to police my speech, accuse me of hatred, call me misogynistic slurs and, above all – as every woman involved in this debate will know – TERF.
If you didn’t already know – and why should you? – ‘TERF’ is an acronym coined by trans activists, which stands for Trans-Exclusionary Radical Feminist. In practice, a huge and diverse cross-section of women are currently being called TERFs and the vast majority have never been radical feminists. Examples of so-called TERFs range from the mother of a gay child who was afraid their child wanted to transition to escape homophobic bullying, to a hitherto totally unfeminist older lady who’s vowed never to visit Marks & Spencer again because they’re allowing any man who says they identify as a woman into the women’s changing rooms. Ironically, radical feminists aren’t even trans-exclusionary – they include trans men in their feminism, because they were born women.
But accusations of TERFery have been sufficient to intimidate many people, institutions and organisations I once admired, who’re cowering before the tactics of the playground. ‘They’ll call us transphobic!’ ‘They’ll say I hate trans people!’ What next, they’ll say you’ve got fleas? Speaking as a biological woman, a lot of people in positions of power really need to grow a pair (which is doubtless literally possible, according to the kind of people who argue that clownfish prove humans aren’t a dimorphic species).
So why am I doing this? Why speak up? Why not quietly do my research and keep my head down?
Well, I’ve got five reasons for being worried about the new trans activism, and deciding I need to speak up.
Firstly, I have a charitable trust that focuses on alleviating social deprivation in Scotland, with a particular emphasis on women and children. Among other things, my trust supports projects for female prisoners and for survivors of domestic and sexual abuse. I also fund medical research into MS, a disease that behaves very differently in men and women. It’s been clear to me for a while that the new trans activism is having (or is likely to have, if all its demands are met) a significant impact on many of the causes I support, because it’s pushing to erode the legal definition of sex and replace it with gender.
The second reason is that I’m an ex-teacher and the founder of a children’s charity, which gives me an interest in both education and safeguarding. Like many others, I have deep concerns about the effect the trans rights movement is having on both.
The third is that, as a much-banned author, I’m interested in freedom of speech and have publicly defended it, even unto Donald Trump.
The fourth is where things start to get truly personal. I’m concerned about the huge explosion in young women wishing to transition and also about the increasing numbers who seem to be detransitioning (returning to their original sex), because they regret taking steps that have, in some cases, altered their bodies irrevocably, and taken away their fertility. Some say they decided to transition after realising they were same-sex attracted, and that transitioning was partly driven by homophobia, either in society or in their families.
Most people probably aren’t aware – I certainly wasn’t, until I started researching this issue properly – that ten years ago, the majority of people wanting to transition to the opposite sex were male. That ratio has now reversed. The UK has experienced a 4400% increase in girls being referred for transitioning treatment. Autistic girls are hugely overrepresented in their numbers.
The same phenomenon has been seen in the US. In 2018, American physician and researcher Lisa Littman set out to explore it. In an interview, she said:
‘Parents online were describing a very unusual pattern of transgender-identification where multiple friends and even entire friend groups became transgender-identified at the same time. I would have been remiss had I not considered social contagion and peer influences as potential factors.’
Littman mentioned Tumblr, Reddit, Instagram and YouTube as contributing factors to Rapid Onset Gender Dysphoria, where she believes that in the realm of transgender identification ‘youth have created particularly insular echo chambers.’
Her paper caused a furore. She was accused of bias and of spreading misinformation about transgender people, subjected to a tsunami of abuse and a concerted campaign to discredit both her and her work. The journal took the paper offline and re-reviewed it before republishing it. However, her career took a similar hit to that suffered by Maya Forstater. Lisa Littman had dared challenge one of the central tenets of trans activism, which is that a person’s gender identity is innate, like sexual orientation. Nobody, the activists insisted, could ever be persuaded into being trans.
The argument of many current trans activists is that if you don’t let a gender dysphoric teenager transition, they will kill themselves. In an article explaining why he resigned from the Tavistock (an NHS gender clinic in England) psychiatrist Marcus Evans stated that claims that children will kill themselves if not permitted to transition do not ‘align substantially with any robust data or studies in this area. Nor do they align with the cases I have encountered over decades as a psychotherapist.’
The writings of young trans men reveal a group of notably sensitive and clever people. The more of their accounts of gender dysphoria I’ve read, with their insightful descriptions of anxiety, dissociation, eating disorders, self-harm and self-hatred, the more I’ve wondered whether, if I’d been born 30 years later, I too might have tried to transition. The allure of escaping womanhood would have been huge. I struggled with severe OCD as a teenager. If I’d found community and sympathy online that I couldn’t find in my immediate environment, I believe I could have been persuaded to turn myself into the son my father had openly said he’d have preferred.
When I read about the theory of gender identity, I remember how mentally sexless I felt in youth. I remember Colette’s description of herself as a ‘mental hermaphrodite’ and Simone de Beauvoir’s words: ‘It is perfectly natural for the future woman to feel indignant at the limitations posed upon her by her sex. The real question is not why she should reject them: the problem is rather to understand why she accepts them.’
As I didn’t have a realistic possibility of becoming a man back in the 1980s, it had to be books and music that got me through both my mental health issues and the sexualised scrutiny and judgement that sets so many girls to war against their bodies in their teens. Fortunately for me, I found my own sense of otherness, and my ambivalence about being a woman, reflected in the work of female writers and musicians who reassured me that, in spite of everything a sexist world tries to throw at the female-bodied, it’s fine not to feel pink, frilly and compliant inside your own head; it’s OK to feel confused, dark, both sexual and non-sexual, unsure of what or who you are.
I want to be very clear here: I know transition will be a solution for some gender dysphoric people, although I’m also aware through extensive research that studies have consistently shown that between 60-90% of gender dysphoric teens will grow out of their dysphoria. Again and again I’ve been told to ‘just meet some trans people.’ I have: in addition to a few younger people, who were all adorable, I happen to know a self-described transsexual woman who’s older than I am and wonderful. Although she’s open about her past as a gay man, I’ve always found it hard to think of her as anything other than a woman, and I believe (and certainly hope) she’s completely happy to have transitioned. Being older, though, she went through a long and rigorous process of evaluation, psychotherapy and staged transformation. The current explosion of trans activism is urging a removal of almost all the robust systems through which candidates for sex reassignment were once required to pass. A man who intends to have no surgery and take no hormones may now secure himself a Gender Recognition Certificate and be a woman in the sight of the law. Many people aren’t aware of this.
We’re living through the most misogynistic period I’ve experienced. Back in the 80s, I imagined that my future daughters, should I have any, would have it far better than I ever did, but between the backlash against feminism and a porn-saturated online culture, I believe things have got significantly worse for girls. Never have I seen women denigrated and dehumanised to the extent they are now. From the leader of the free world’s long history of sexual assault accusations and his proud boast of ‘grabbing them by the pussy’, to the incel (‘involuntarily celibate’) movement that rages against women who won’t give them sex, to the trans activists who declare that TERFs need punching and re-educating, men across the political spectrum seem to agree: women are asking for trouble. Everywhere, women are being told to shut up and sit down, or else.
I’ve read all the arguments about femaleness not residing in the sexed body, and the assertions that biological women don’t have common experiences, and I find them, too, deeply misogynistic and regressive. It’s also clear that one of the objectives of denying the importance of sex is to erode what some seem to see as the cruelly segregationist idea of women having their own biological realities or – just as threatening – unifying realities that make them a cohesive political class. The hundreds of emails I’ve received in the last few days prove this erosion concerns many others just as much. It isn’t enough for women to be trans allies. Women must accept and admit that there is no material difference between trans women and themselves.
But, as many women have said before me, ‘woman’ is not a costume. ‘Woman’ is not an idea in a man’s head. ‘Woman’ is not a pink brain, a liking for Jimmy Choos or any of the other sexist ideas now somehow touted as progressive. Moreover, the ‘inclusive’ language that calls female people ‘menstruators’ and ‘people with vulvas’ strikes many women as dehumanising and demeaning. I understand why trans activists consider this language to be appropriate and kind, but for those of us who’ve had degrading slurs spat at us by violent men, it’s not neutral, it’s hostile and alienating.
Which brings me to the fifth reason I’m deeply concerned about the consequences of the current trans activism.
I’ve been in the public eye now for over twenty years and have never talked publicly about being a domestic abuse and sexual assault survivor. This isn’t because I’m ashamed those things happened to me, but because they’re traumatic to revisit and remember. I also feel protective of my daughter from my first marriage. I didn’t want to claim sole ownership of a story that belongs to her, too. However, a short while ago, I asked her how she’d feel if I were publicly honest about that part of my life, and she encouraged me to go ahead.
I’m mentioning these things now not in an attempt to garner sympathy, but out of solidarity with the huge numbers of women who have histories like mine, who’ve been slurred as bigots for having concerns around single-sex spaces.
I managed to escape my first violent marriage with some difficulty, but I’m now married to a truly good and principled man, safe and secure in ways I never in a million years expected to be. However, the scars left by violence and sexual assault don’t disappear, no matter how loved you are, and no matter how much money you’ve made. My perennial jumpiness is a family joke – and even I know it’s funny – but I pray my daughters never have the same reasons I do for hating sudden loud noises, or finding people behind me when I haven’t heard them approaching.
If you could come inside my head and understand what I feel when I read about a trans woman dying at the hands of a violent man, you’d find solidarity and kinship. I have a visceral sense of the terror in which those trans women will have spent their last seconds on earth, because I too have known moments of blind fear when I realised that the only thing keeping me alive was the shaky self-restraint of my attacker.
I believe the majority of trans-identified people not only pose zero threat to others, but are vulnerable for all the reasons I’ve outlined. Trans people need and deserve protection. Like women, they’re most likely to be killed by sexual partners. Trans women who work in the sex industry, particularly trans women of colour, are at particular risk. Like every other domestic abuse and sexual assault survivor I know, I feel nothing but empathy and solidarity with trans women who’ve been abused by men.
So I want trans women to be safe. At the same time, I do not want to make natal girls and women less safe. When you throw open the doors of bathrooms and changing rooms to any man who believes or feels he’s a woman – and, as I’ve said, gender confirmation certificates may now be granted without any need for surgery or hormones – then you open the door to any and all men who wish to come inside. That is the simple truth.
On Saturday morning, I read that the Scottish government is proceeding with its controversial gender recognition plans, which will in effect mean that all a man needs to ‘become a woman’ is to say he’s one. To use a very contemporary word, I was ‘triggered’. Ground down by the relentless attacks from trans activists on social media, when I was only there to give children feedback about pictures they’d drawn for my book under lockdown, I spent much of Saturday in a very dark place inside my head, as memories of a serious sexual assault I suffered in my twenties recurred on a loop. That assault happened at a time and in a space where I was vulnerable, and a man capitalised on an opportunity. I couldn’t shut out those memories and I was finding it hard to contain my anger and disappointment about the way I believe my government is playing fast and loose with womens and girls’ safety.
Late on Saturday evening, scrolling through children’s pictures before I went to bed, I forgot the first rule of Twitter – never, ever expect a nuanced conversation – and reacted to what I felt was degrading language about women. I spoke up about the importance of sex and have been paying the price ever since. I was transphobic, I was a cunt, a bitch, a TERF, I deserved cancelling, punching and death. You are Voldemort said one person, clearly feeling this was the only language I’d understand.
It would be so much easier to tweet the approved hashtags – because of course trans rights are human rights and of course trans lives matter – scoop up the woke cookies and bask in a virtue-signalling afterglow. There’s joy, relief and safety in conformity. As Simone de Beauvoir also wrote, “… without a doubt it is more comfortable to endure blind bondage than to work for one’s liberation; the dead, too, are better suited to the earth than the living.”
Huge numbers of women are justifiably terrified by the trans activists; I know this because so many have got in touch with me to tell their stories. They’re afraid of doxxing, of losing their jobs or their livelihoods, and of violence.
But endlessly unpleasant as its constant targeting of me has been, I refuse to bow down to a movement that I believe is doing demonstrable harm in seeking to erode ‘woman’ as a political and biological class and offering cover to predators like few before it. I stand alongside the brave women and men, gay, straight and trans, who’re standing up for freedom of speech and thought, and for the rights and safety of some of the most vulnerable in our society: young gay kids, fragile teenagers, and women who’re reliant on and wish to retain their single sex spaces. Polls show those women are in the vast majority, and exclude only those privileged or lucky enough never to have come up against male violence or sexual assault, and who’ve never troubled to educate themselves on how prevalent it is.
The one thing that gives me hope is that the women who can protest and organise, are doing so, and they have some truly decent men and trans people alongside them. Political parties seeking to appease the loudest voices in this debate are ignoring women’s concerns at their peril. In the UK, women are reaching out to each other across party lines, concerned about the erosion of their hard-won rights and widespread intimidation. None of the gender critical women I’ve talked to hates trans people; on the contrary. Many of them became interested in this issue in the first place out of concern for trans youth, and they’re hugely sympathetic towards trans adults who simply want to live their lives, but who’re facing a backlash for a brand of activism they don’t endorse. The supreme irony is that the attempt to silence women with the word ‘TERF’ may have pushed more young women towards radical feminism than the movement’s seen in decades.
The last thing I want to say is this. I haven’t written this essay in the hope that anybody will get out a violin for me, not even a teeny-weeny one. I’m extraordinarily fortunate; I’m a survivor, certainly not a victim. I’ve only mentioned my past because, like every other human being on this planet, I have a complex backstory, which shapes my fears, my interests and my opinions. I never forget that inner complexity when I’m creating a fictional character and I certainly never forget it when it comes to trans people.
All I’m asking – all I want – is for similar empathy, similar understanding, to be extended to the many millions of women whose sole crime is wanting their concerns to be heard without receiving threats and abuse.
I’d stepped back from Twitter for many months both before and after tweeting support for Maya, because I knew it was doing nothing good for my mental health. I only returned because I wanted to share a free children’s book during the pandemic. Immediately, activists who clearly believe themselves to be good, kind and progressive people swarmed back into my timeline, assuming a right to police my speech, accuse me of hatred, call me misogynistic slurs and, above all – as every woman involved in this debate will know – TERF.
If you didn’t already know – and why should you? – ‘TERF’ is an acronym coined by trans activists, which stands for Trans-Exclusionary Radical Feminist. In practice, a huge and diverse cross-section of women are currently being called TERFs and the vast majority have never been radical feminists. Examples of so-called TERFs range from the mother of a gay child who was afraid their child wanted to transition to escape homophobic bullying, to a hitherto totally unfeminist older lady who’s vowed never to visit Marks & Spencer again because they’re allowing any man who says they identify as a woman into the women’s changing rooms. Ironically, radical feminists aren’t even trans-exclusionary – they include trans men in their feminism, because they were born women.
But accusations of TERFery have been sufficient to intimidate many people, institutions and organisations I once admired, who’re cowering before the tactics of the playground. ‘They’ll call us transphobic!’ ‘They’ll say I hate trans people!’ What next, they’ll say you’ve got fleas? Speaking as a biological woman, a lot of people in positions of power really need to grow a pair (which is doubtless literally possible, according to the kind of people who argue that clownfish prove humans aren’t a dimorphic species).
So why am I doing this? Why speak up? Why not quietly do my research and keep my head down?
Well, I’ve got five reasons for being worried about the new trans activism, and deciding I need to speak up.
Firstly, I have a charitable trust that focuses on alleviating social deprivation in Scotland, with a particular emphasis on women and children. Among other things, my trust supports projects for female prisoners and for survivors of domestic and sexual abuse. I also fund medical research into MS, a disease that behaves very differently in men and women. It’s been clear to me for a while that the new trans activism is having (or is likely to have, if all its demands are met) a significant impact on many of the causes I support, because it’s pushing to erode the legal definition of sex and replace it with gender.
The second reason is that I’m an ex-teacher and the founder of a children’s charity, which gives me an interest in both education and safeguarding. Like many others, I have deep concerns about the effect the trans rights movement is having on both.
The third is that, as a much-banned author, I’m interested in freedom of speech and have publicly defended it, even unto Donald Trump.
The fourth is where things start to get truly personal. I’m concerned about the huge explosion in young women wishing to transition and also about the increasing numbers who seem to be detransitioning (returning to their original sex), because they regret taking steps that have, in some cases, altered their bodies irrevocably, and taken away their fertility. Some say they decided to transition after realising they were same-sex attracted, and that transitioning was partly driven by homophobia, either in society or in their families.
Most people probably aren’t aware – I certainly wasn’t, until I started researching this issue properly – that ten years ago, the majority of people wanting to transition to the opposite sex were male. That ratio has now reversed. The UK has experienced a 4400% increase in girls being referred for transitioning treatment. Autistic girls are hugely overrepresented in their numbers.
The same phenomenon has been seen in the US. In 2018, American physician and researcher Lisa Littman set out to explore it. In an interview, she said:
‘Parents online were describing a very unusual pattern of transgender-identification where multiple friends and even entire friend groups became transgender-identified at the same time. I would have been remiss had I not considered social contagion and peer influences as potential factors.’
Littman mentioned Tumblr, Reddit, Instagram and YouTube as contributing factors to Rapid Onset Gender Dysphoria, where she believes that in the realm of transgender identification ‘youth have created particularly insular echo chambers.’
Her paper caused a furore. She was accused of bias and of spreading misinformation about transgender people, subjected to a tsunami of abuse and a concerted campaign to discredit both her and her work. The journal took the paper offline and re-reviewed it before republishing it. However, her career took a similar hit to that suffered by Maya Forstater. Lisa Littman had dared challenge one of the central tenets of trans activism, which is that a person’s gender identity is innate, like sexual orientation. Nobody, the activists insisted, could ever be persuaded into being trans.
The argument of many current trans activists is that if you don’t let a gender dysphoric teenager transition, they will kill themselves. In an article explaining why he resigned from the Tavistock (an NHS gender clinic in England) psychiatrist Marcus Evans stated that claims that children will kill themselves if not permitted to transition do not ‘align substantially with any robust data or studies in this area. Nor do they align with the cases I have encountered over decades as a psychotherapist.’
The writings of young trans men reveal a group of notably sensitive and clever people. The more of their accounts of gender dysphoria I’ve read, with their insightful descriptions of anxiety, dissociation, eating disorders, self-harm and self-hatred, the more I’ve wondered whether, if I’d been born 30 years later, I too might have tried to transition. The allure of escaping womanhood would have been huge. I struggled with severe OCD as a teenager. If I’d found community and sympathy online that I couldn’t find in my immediate environment, I believe I could have been persuaded to turn myself into the son my father had openly said he’d have preferred.
When I read about the theory of gender identity, I remember how mentally sexless I felt in youth. I remember Colette’s description of herself as a ‘mental hermaphrodite’ and Simone de Beauvoir’s words: ‘It is perfectly natural for the future woman to feel indignant at the limitations posed upon her by her sex. The real question is not why she should reject them: the problem is rather to understand why she accepts them.’
As I didn’t have a realistic possibility of becoming a man back in the 1980s, it had to be books and music that got me through both my mental health issues and the sexualised scrutiny and judgement that sets so many girls to war against their bodies in their teens. Fortunately for me, I found my own sense of otherness, and my ambivalence about being a woman, reflected in the work of female writers and musicians who reassured me that, in spite of everything a sexist world tries to throw at the female-bodied, it’s fine not to feel pink, frilly and compliant inside your own head; it’s OK to feel confused, dark, both sexual and non-sexual, unsure of what or who you are.
I want to be very clear here: I know transition will be a solution for some gender dysphoric people, although I’m also aware through extensive research that studies have consistently shown that between 60-90% of gender dysphoric teens will grow out of their dysphoria. Again and again I’ve been told to ‘just meet some trans people.’ I have: in addition to a few younger people, who were all adorable, I happen to know a self-described transsexual woman who’s older than I am and wonderful. Although she’s open about her past as a gay man, I’ve always found it hard to think of her as anything other than a woman, and I believe (and certainly hope) she’s completely happy to have transitioned. Being older, though, she went through a long and rigorous process of evaluation, psychotherapy and staged transformation. The current explosion of trans activism is urging a removal of almost all the robust systems through which candidates for sex reassignment were once required to pass. A man who intends to have no surgery and take no hormones may now secure himself a Gender Recognition Certificate and be a woman in the sight of the law. Many people aren’t aware of this.
We’re living through the most misogynistic period I’ve experienced. Back in the 80s, I imagined that my future daughters, should I have any, would have it far better than I ever did, but between the backlash against feminism and a porn-saturated online culture, I believe things have got significantly worse for girls. Never have I seen women denigrated and dehumanised to the extent they are now. From the leader of the free world’s long history of sexual assault accusations and his proud boast of ‘grabbing them by the pussy’, to the incel (‘involuntarily celibate’) movement that rages against women who won’t give them sex, to the trans activists who declare that TERFs need punching and re-educating, men across the political spectrum seem to agree: women are asking for trouble. Everywhere, women are being told to shut up and sit down, or else.
I’ve read all the arguments about femaleness not residing in the sexed body, and the assertions that biological women don’t have common experiences, and I find them, too, deeply misogynistic and regressive. It’s also clear that one of the objectives of denying the importance of sex is to erode what some seem to see as the cruelly segregationist idea of women having their own biological realities or – just as threatening – unifying realities that make them a cohesive political class. The hundreds of emails I’ve received in the last few days prove this erosion concerns many others just as much. It isn’t enough for women to be trans allies. Women must accept and admit that there is no material difference between trans women and themselves.
But, as many women have said before me, ‘woman’ is not a costume. ‘Woman’ is not an idea in a man’s head. ‘Woman’ is not a pink brain, a liking for Jimmy Choos or any of the other sexist ideas now somehow touted as progressive. Moreover, the ‘inclusive’ language that calls female people ‘menstruators’ and ‘people with vulvas’ strikes many women as dehumanising and demeaning. I understand why trans activists consider this language to be appropriate and kind, but for those of us who’ve had degrading slurs spat at us by violent men, it’s not neutral, it’s hostile and alienating.
Which brings me to the fifth reason I’m deeply concerned about the consequences of the current trans activism.
I’ve been in the public eye now for over twenty years and have never talked publicly about being a domestic abuse and sexual assault survivor. This isn’t because I’m ashamed those things happened to me, but because they’re traumatic to revisit and remember. I also feel protective of my daughter from my first marriage. I didn’t want to claim sole ownership of a story that belongs to her, too. However, a short while ago, I asked her how she’d feel if I were publicly honest about that part of my life, and she encouraged me to go ahead.
I’m mentioning these things now not in an attempt to garner sympathy, but out of solidarity with the huge numbers of women who have histories like mine, who’ve been slurred as bigots for having concerns around single-sex spaces.
I managed to escape my first violent marriage with some difficulty, but I’m now married to a truly good and principled man, safe and secure in ways I never in a million years expected to be. However, the scars left by violence and sexual assault don’t disappear, no matter how loved you are, and no matter how much money you’ve made. My perennial jumpiness is a family joke – and even I know it’s funny – but I pray my daughters never have the same reasons I do for hating sudden loud noises, or finding people behind me when I haven’t heard them approaching.
If you could come inside my head and understand what I feel when I read about a trans woman dying at the hands of a violent man, you’d find solidarity and kinship. I have a visceral sense of the terror in which those trans women will have spent their last seconds on earth, because I too have known moments of blind fear when I realised that the only thing keeping me alive was the shaky self-restraint of my attacker.
I believe the majority of trans-identified people not only pose zero threat to others, but are vulnerable for all the reasons I’ve outlined. Trans people need and deserve protection. Like women, they’re most likely to be killed by sexual partners. Trans women who work in the sex industry, particularly trans women of colour, are at particular risk. Like every other domestic abuse and sexual assault survivor I know, I feel nothing but empathy and solidarity with trans women who’ve been abused by men.
So I want trans women to be safe. At the same time, I do not want to make natal girls and women less safe. When you throw open the doors of bathrooms and changing rooms to any man who believes or feels he’s a woman – and, as I’ve said, gender confirmation certificates may now be granted without any need for surgery or hormones – then you open the door to any and all men who wish to come inside. That is the simple truth.
On Saturday morning, I read that the Scottish government is proceeding with its controversial gender recognition plans, which will in effect mean that all a man needs to ‘become a woman’ is to say he’s one. To use a very contemporary word, I was ‘triggered’. Ground down by the relentless attacks from trans activists on social media, when I was only there to give children feedback about pictures they’d drawn for my book under lockdown, I spent much of Saturday in a very dark place inside my head, as memories of a serious sexual assault I suffered in my twenties recurred on a loop. That assault happened at a time and in a space where I was vulnerable, and a man capitalised on an opportunity. I couldn’t shut out those memories and I was finding it hard to contain my anger and disappointment about the way I believe my government is playing fast and loose with womens and girls’ safety.
Late on Saturday evening, scrolling through children’s pictures before I went to bed, I forgot the first rule of Twitter – never, ever expect a nuanced conversation – and reacted to what I felt was degrading language about women. I spoke up about the importance of sex and have been paying the price ever since. I was transphobic, I was a cunt, a bitch, a TERF, I deserved cancelling, punching and death. You are Voldemort said one person, clearly feeling this was the only language I’d understand.
It would be so much easier to tweet the approved hashtags – because of course trans rights are human rights and of course trans lives matter – scoop up the woke cookies and bask in a virtue-signalling afterglow. There’s joy, relief and safety in conformity. As Simone de Beauvoir also wrote, “… without a doubt it is more comfortable to endure blind bondage than to work for one’s liberation; the dead, too, are better suited to the earth than the living.”
Huge numbers of women are justifiably terrified by the trans activists; I know this because so many have got in touch with me to tell their stories. They’re afraid of doxxing, of losing their jobs or their livelihoods, and of violence.
But endlessly unpleasant as its constant targeting of me has been, I refuse to bow down to a movement that I believe is doing demonstrable harm in seeking to erode ‘woman’ as a political and biological class and offering cover to predators like few before it. I stand alongside the brave women and men, gay, straight and trans, who’re standing up for freedom of speech and thought, and for the rights and safety of some of the most vulnerable in our society: young gay kids, fragile teenagers, and women who’re reliant on and wish to retain their single sex spaces. Polls show those women are in the vast majority, and exclude only those privileged or lucky enough never to have come up against male violence or sexual assault, and who’ve never troubled to educate themselves on how prevalent it is.
The one thing that gives me hope is that the women who can protest and organise, are doing so, and they have some truly decent men and trans people alongside them. Political parties seeking to appease the loudest voices in this debate are ignoring women’s concerns at their peril. In the UK, women are reaching out to each other across party lines, concerned about the erosion of their hard-won rights and widespread intimidation. None of the gender critical women I’ve talked to hates trans people; on the contrary. Many of them became interested in this issue in the first place out of concern for trans youth, and they’re hugely sympathetic towards trans adults who simply want to live their lives, but who’re facing a backlash for a brand of activism they don’t endorse. The supreme irony is that the attempt to silence women with the word ‘TERF’ may have pushed more young women towards radical feminism than the movement’s seen in decades.
The last thing I want to say is this. I haven’t written this essay in the hope that anybody will get out a violin for me, not even a teeny-weeny one. I’m extraordinarily fortunate; I’m a survivor, certainly not a victim. I’ve only mentioned my past because, like every other human being on this planet, I have a complex backstory, which shapes my fears, my interests and my opinions. I never forget that inner complexity when I’m creating a fictional character and I certainly never forget it when it comes to trans people.
All I’m asking – all I want – is for similar empathy, similar understanding, to be extended to the many millions of women whose sole crime is wanting their concerns to be heard without receiving threats and abuse.
I’d stepped back from Twitter for many months both before and after tweeting support for Maya, because I knew it was doing nothing good for my mental health. I only returned because I wanted to share a free children’s book during the pandemic. Immediately, activists who clearly believe themselves to be good, kind and progressive people swarmed back into my timeline, assuming a right to police my speech, accuse me of hatred, call me misogynistic slurs and, above all – as every woman involved in this debate will know – TERF.
If you didn’t already know – and why should you? – ‘TERF’ is an acronym coined by trans activists, which stands for Trans-Exclusionary Radical Feminist. In practice, a huge and diverse cross-section of women are currently being called TERFs and the vast majority have never been radical feminists. Examples of so-called TERFs range from the mother of a gay child who was afraid their child wanted to transition to escape homophobic bullying, to a hitherto totally unfeminist older lady who’s vowed never to visit Marks & Spencer again because they’re allowing any man who says they identify as a woman into the women’s changing rooms. Ironically, radical feminists aren’t even trans-exclusionary – they include trans men in their feminism, because they were born women.
But accusations of TERFery have been sufficient to intimidate many people, institutions and organisations I once admired, who’re cowering before the tactics of the playground. ‘They’ll call us transphobic!’ ‘They’ll say I hate trans people!’ What next, they’ll say you’ve got fleas? Speaking as a biological woman, a lot of people in positions of power really need to grow a pair (which is doubtless literally possible, according to the kind of people who argue that clownfish prove humans aren’t a dimorphic species).
So why am I doing this? Why speak up? Why not quietly do my research and keep my head down?
Well, I’ve got five reasons for being worried about the new trans activism, and deciding I need to speak up.
Firstly, I have a charitable trust that focuses on alleviating social deprivation in Scotland, with a particular emphasis on women and children. Among other things, my trust supports projects for female prisoners and for survivors of domestic and sexual abuse. I also fund medical research into MS, a disease that behaves very differently in men and women. It’s been clear to me for a while that the new trans activism is having (or is likely to have, if all its demands are met) a significant impact on many of the causes I support, because it’s pushing to erode the legal definition of sex and replace it with gender.
The second reason is that I’m an ex-teacher and the founder of a children’s charity, which gives me an interest in both education and safeguarding. Like many others, I have deep concerns about the effect the trans rights movement is having on both.
The third is that, as a much-banned author, I’m interested in freedom of speech and have publicly defended it, even unto Donald Trump.
The fourth is where things start to get truly personal. I’m concerned about the huge explosion in young women wishing to transition and also about the increasing numbers who seem to be detransitioning (returning to their original sex), because they regret taking steps that have, in some cases, altered their bodies irrevocably, and taken away their fertility. Some say they decided to transition after realising they were same-sex attracted, and that transitioning was partly driven by homophobia, either in society or in their families.
Most people probably aren’t aware – I certainly wasn’t, until I started researching this issue properly – that ten years ago, the majority of people wanting to transition to the opposite sex were male. That ratio has now reversed. The UK has experienced a 4400% increase in girls being referred for transitioning treatment. Autistic girls are hugely overrepresented in their numbers.
The same phenomenon has been seen in the US. In 2018, American physician and researcher Lisa Littman set out to explore it. In an interview, she said:
‘Parents online were describing a very unusual pattern of transgender-identification where multiple friends and even entire friend groups became transgender-identified at the same time. I would have been remiss had I not considered social contagion and peer influences as potential factors.’
Littman mentioned Tumblr, Reddit, Instagram and YouTube as contributing factors to Rapid Onset Gender Dysphoria, where she believes that in the realm of transgender identification ‘youth have created particularly insular echo chambers.’
Her paper caused a furore. She was accused of bias and of spreading misinformation about transgender people, subjected to a tsunami of abuse and a concerted campaign to discredit both her and her work. The journal took the paper offline and re-reviewed it before republishing it. However, her career took a similar hit to that suffered by Maya Forstater. Lisa Littman had dared challenge one of the central tenets of trans activism, which is that a person’s gender identity is innate, like sexual orientation. Nobody, the activists insisted, could ever be persuaded into being trans.
The argument of many current trans activists is that if you don’t let a gender dysphoric teenager transition, they will kill themselves. In an article explaining why he resigned from the Tavistock (an NHS gender clinic in England) psychiatrist Marcus Evans stated that claims that children will kill themselves if not permitted to transition do not ‘align substantially with any robust data or studies in this area. Nor do they align with the cases I have encountered over decades as a psychotherapist.’
The writings of young trans men reveal a group of notably sensitive and clever people. The more of their accounts of gender dysphoria I’ve read, with their insightful descriptions of anxiety, dissociation, eating disorders, self-harm and self-hatred, the more I’ve wondered whether, if I’d been born 30 years later, I too might have tried to transition. The allure of escaping womanhood would have been huge. I struggled with severe OCD as a teenager. If I’d found community and sympathy online that I couldn’t find in my immediate environment, I believe I could have been persuaded to turn myself into the son my father had openly said he’d have preferred.
When I read about the theory of gender identity, I remember how mentally sexless I felt in youth. I remember Colette’s description of herself as a ‘mental hermaphrodite’ and Simone de Beauvoir’s words: ‘It is perfectly natural for the future woman to feel indignant at the limitations posed upon her by her sex. The real question is not why she should reject them: the problem is rather to understand why she accepts them.’
As I didn’t have a realistic possibility of becoming a man back in the 1980s, it had to be books and music that got me through both my mental health issues and the sexualised scrutiny and judgement that sets so many girls to war against their bodies in their teens. Fortunately for me, I found my own sense of otherness, and my ambivalence about being a woman, reflected in the work of female writers and musicians who reassured me that, in spite of everything a sexist world tries to throw at the female-bodied, it’s fine not to feel pink, frilly and compliant inside your own head; it’s OK to feel confused, dark, both sexual and non-sexual, unsure of what or who you are.
I want to be very clear here: I know transition will be a solution for some gender dysphoric people, although I’m also aware through extensive research that studies have consistently shown that between 60-90% of gender dysphoric teens will grow out of their dysphoria. Again and again I’ve been told to ‘just meet some trans people.’ I have: in addition to a few younger people, who were all adorable, I happen to know a self-described transsexual woman who’s older than I am and wonderful. Although she’s open about her past as a gay man, I’ve always found it hard to think of her as anything other than a woman, and I believe (and certainly hope) she’s completely happy to have transitioned. Being older, though, she went through a long and rigorous process of evaluation, psychotherapy and staged transformation. The current explosion of trans activism is urging a removal of almost all the robust systems through which candidates for sex reassignment were once required to pass. A man who intends to have no surgery and take no hormones may now secure himself a Gender Recognition Certificate and be a woman in the sight of the law. Many people aren’t aware of this.
We’re living through the most misogynistic period I’ve experienced. Back in the 80s, I imagined that my future daughters, should I have any, would have it far better than I ever did, but between the backlash against feminism and a porn-saturated online culture, I believe things have got significantly worse for girls. Never have I seen women denigrated and dehumanised to the extent they are now. From the leader of the free world’s long history of sexual assault accusations and his proud boast of ‘grabbing them by the pussy’, to the incel (‘involuntarily celibate’) movement that rages against women who won’t give them sex, to the trans activists who declare that TERFs need punching and re-educating, men across the political spectrum seem to agree: women are asking for trouble. Everywhere, women are being told to shut up and sit down, or else.
I’ve read all the arguments about femaleness not residing in the sexed body, and the assertions that biological women don’t have common experiences, and I find them, too, deeply misogynistic and regressive. It’s also clear that one of the objectives of denying the importance of sex is to erode what some seem to see as the cruelly segregationist idea of women having their own biological realities or – just as threatening – unifying realities that make them a cohesive political class. The hundreds of emails I’ve received in the last few days prove this erosion concerns many others just as much. It isn’t enough for women to be trans allies. Women must accept and admit that there is no material difference between trans women and themselves.
But, as many women have said before me, ‘woman’ is not a costume. ‘Woman’ is not an idea in a man’s head. ‘Woman’ is not a pink brain, a liking for Jimmy Choos or any of the other sexist ideas now somehow touted as progressive. Moreover, the ‘inclusive’ language that calls female people ‘menstruators’ and ‘people with vulvas’ strikes many women as dehumanising and demeaning. I understand why trans activists consider this language to be appropriate and kind, but for those of us who’ve had degrading slurs spat at us by violent men, it’s not neutral, it’s hostile and alienating.
Which brings me to the fifth reason I’m deeply concerned about the consequences of the current trans activism.
I’ve been in the public eye now for over twenty years and have never talked publicly about being a domestic abuse and sexual assault survivor. This isn’t because I’m ashamed those things happened to me, but because they’re traumatic to revisit and remember. I also feel protective of my daughter from my first marriage. I didn’t want to claim sole ownership of a story that belongs to her, too. However, a short while ago, I asked her how she’d feel if I were publicly honest about that part of my life, and she encouraged me to go ahead.
I’m mentioning these things now not in an attempt to garner sympathy, but out of solidarity with the huge numbers of women who have histories like mine, who’ve been slurred as bigots for having concerns around single-sex spaces.
I managed to escape my first violent marriage with some difficulty, but I’m now married to a truly good and principled man, safe and secure in ways I never in a million years expected to be. However, the scars left by violence and sexual assault don’t disappear, no matter how loved you are, and no matter how much money you’ve made. My perennial jumpiness is a family joke – and even I know it’s funny – but I pray my daughters never have the same reasons I do for hating sudden loud noises, or finding people behind me when I haven’t heard them approaching.
If you could come inside my head and understand what I feel when I read about a trans woman dying at the hands of a violent man, you’d find solidarity and kinship. I have a visceral sense of the terror in which those trans women will have spent their last seconds on earth, because I too have known moments of blind fear when I realised that the only thing keeping me alive was the shaky self-restraint of my attacker.
I believe the majority of trans-identified people not only pose zero threat to others, but are vulnerable for all the reasons I’ve outlined. Trans people need and deserve protection. Like women, they’re most likely to be killed by sexual partners. Trans women who work in the sex industry, particularly trans women of colour, are at particular risk. Like every other domestic abuse and sexual assault survivor I know, I feel nothing but empathy and solidarity with trans women who’ve been abused by men.
So I want trans women to be safe. At the same time, I do not want to make natal girls and women less safe. When you throw open the doors of bathrooms and changing rooms to any man who believes or feels he’s a woman – and, as I’ve said, gender confirmation certificates may now be granted without any need for surgery or hormones – then you open the door to any and all men who wish to come inside. That is the simple truth.
On Saturday morning, I read that the Scottish government is proceeding with its controversial gender recognition plans, which will in effect mean that all a man needs to ‘become a woman’ is to say he’s one. To use a very contemporary word, I was ‘triggered’. Ground down by the relentless attacks from trans activists on social media, when I was only there to give children feedback about pictures they’d drawn for my book under lockdown, I spent much of Saturday in a very dark place inside my head, as memories of a serious sexual assault I suffered in my twenties recurred on a loop. That assault happened at a time and in a space where I was vulnerable, and a man capitalised on an opportunity. I couldn’t shut out those memories and I was finding it hard to contain my anger and disappointment about the way I believe my government is playing fast and loose with womens and girls’ safety.
Late on Saturday evening, scrolling through children’s pictures before I went to bed, I forgot the first rule of Twitter – never, ever expect a nuanced conversation – and reacted to what I felt was degrading language about women. I spoke up about the importance of sex and have been paying the price ever since. I was transphobic, I was a cunt, a bitch, a TERF, I deserved cancelling, punching and death. You are Voldemort said one person, clearly feeling this was the only language I’d understand.
It would be so much easier to tweet the approved hashtags – because of course trans rights are human rights and of course trans lives matter – scoop up the woke cookies and bask in a virtue-signalling afterglow. There’s joy, relief and safety in conformity. As Simone de Beauvoir also wrote, “… without a doubt it is more comfortable to endure blind bondage than to work for one’s liberation; the dead, too, are better suited to the earth than the living.”
Huge numbers of women are justifiably terrified by the trans activists; I know this because so many have got in touch with me to tell their stories. They’re afraid of doxxing, of losing their jobs or their livelihoods, and of violence.
But endlessly unpleasant as its constant targeting of me has been, I refuse to bow down to a movement that I believe is doing demonstrable harm in seeking to erode ‘woman’ as a political and biological class and offering cover to predators like few before it. I stand alongside the brave women and men, gay, straight and trans, who’re standing up for freedom of speech and thought, and for the rights and safety of some of the most vulnerable in our society: young gay kids, fragile teenagers, and women who’re reliant on and wish to retain their single sex spaces. Polls show those women are in the vast majority, and exclude only those privileged or lucky enough never to have come up against male violence or sexual assault, and who’ve never troubled to educate themselves on how prevalent it is.
The one thing that gives me hope is that the women who can protest and organise, are doing so, and they have some truly decent men and trans people alongside them. Political parties seeking to appease the loudest voices in this debate are ignoring women’s concerns at their peril. In the UK, women are reaching out to each other across party lines, concerned about the erosion of their hard-won rights and widespread intimidation. None of the gender critical women I’ve talked to hates trans people; on the contrary. Many of them became interested in this issue in the first place out of concern for trans youth, and they’re hugely sympathetic towards trans adults who simply want to live their lives, but who’re facing a backlash for a brand of activism they don’t endorse. The supreme irony is that the attempt to silence women with the word ‘TERF’ may have pushed more young women towards radical feminism than the movement’s seen in decades.
The last thing I want to say is this. I haven’t written this essay in the hope that anybody will get out a violin for me, not even a teeny-weeny one. I’m extraordinarily fortunate; I’m a survivor, certainly not a victim. I’ve only mentioned my past because, like every other human being on this planet, I have a complex backstory, which shapes my fears, my interests and my opinions. I never forget that inner complexity when I’m creating a fictional character and I certainly never forget it when it comes to trans people.
All I’m asking – all I want – is for similar empathy, similar understanding, to be extended to the many millions of women whose sole crime is wanting their concerns to be heard without receiving threats and abuse.
All I’m asking – all I want – is for similar empathy, similar understanding, to be extended to the many millions of women whose sole crime is wanting their concerns to be heard without receiving threats and abuse.
I’d stepped back from Twitter for many months both before and after tweeting support for Maya, because I knew it was doing nothing good for my mental health. I only returned because I wanted to share a free children’s book during the pandemic. Immediately, activists who clearly believe themselves to be good, kind and progressive people swarmed back into my timeline, assuming a right to police my speech, accuse me of hatred, call me misogynistic slurs and, above all – as every woman involved in this debate will know – TERF.
If you didn’t already know – and why should you? – ‘TERF’ is an acronym coined by trans activists, which stands for Trans-Exclusionary Radical Feminist. In practice, a huge and diverse cross-section of women are currently being called TERFs and the vast majority have never been radical feminists. Examples of so-called TERFs range from the mother of a gay child who was afraid their child wanted to transition to escape homophobic bullying, to a hitherto totally unfeminist older lady who’s vowed never to visit Marks & Spencer again because they’re allowing any man who says they identify as a woman into the women’s changing rooms. Ironically, radical feminists aren’t even trans-exclusionary – they include trans men in their feminism, because they were born women.
But accusations of TERFery have been sufficient to intimidate many people, institutions and organisations I once admired, who’re cowering before the tactics of the playground. ‘They’ll call us transphobic!’ ‘They’ll say I hate trans people!’ What next, they’ll say you’ve got fleas? Speaking as a biological woman, a lot of people in positions of power really need to grow a pair (which is doubtless literally possible, according to the kind of people who argue that clownfish prove humans aren’t a dimorphic species).
So why am I doing this? Why speak up? Why not quietly do my research and keep my head down?
Well, I’ve got five reasons for being worried about the new trans activism, and deciding I need to speak up.
Firstly, I have a charitable trust that focuses on alleviating social deprivation in Scotland, with a particular emphasis on women and children. Among other things, my trust supports projects for female prisoners and for survivors of domestic and sexual abuse. I also fund medical research into MS, a disease that behaves very differently in men and women. It’s been clear to me for a while that the new trans activism is having (or is likely to have, if all its demands are met) a significant impact on many of the causes I support, because it’s pushing to erode the legal definition of sex and replace it with gender.
The second reason is that I’m an ex-teacher and the founder of a children’s charity, which gives me an interest in both education and safeguarding. Like many others, I have deep concerns about the effect the trans rights movement is having on both.
The third is that, as a much-banned author, I’m interested in freedom of speech and have publicly defended it, even unto Donald Trump.
The fourth is where things start to get truly personal. I’m concerned about the huge explosion in young women wishing to transition and also about the increasing numbers who seem to be detransitioning (returning to their original sex), because they regret taking steps that have, in some cases, altered their bodies irrevocably, and taken away their fertility. Some say they decided to transition after realising they were same-sex attracted, and that transitioning was partly driven by homophobia, either in society or in their families.
Most people probably aren’t aware – I certainly wasn’t, until I started researching this issue properly – that ten years ago, the majority of people wanting to transition to the opposite sex were male. That ratio has now reversed. The UK has experienced a 4400% increase in girls being referred for transitioning treatment. Autistic girls are hugely overrepresented in their numbers.
The same phenomenon has been seen in the US. In 2018, American physician and researcher Lisa Littman set out to explore it. In an interview, she said:
‘Parents online were describing a very unusual pattern of transgender-identification where multiple friends and even entire friend groups became transgender-identified at the same time. I would have been remiss had I not considered social contagion and peer influences as potential factors.’
Littman mentioned Tumblr, Reddit, Instagram and YouTube as contributing factors to Rapid Onset Gender Dysphoria, where she believes that in the realm of transgender identification ‘youth have created particularly insular echo chambers.’
Her paper caused a furore. She was accused of bias and of spreading misinformation about transgender people, subjected to a tsunami of abuse and a concerted campaign to discredit both her and her work. The journal took the paper offline and re-reviewed it before republishing it. However, her career took a similar hit to that suffered by Maya Forstater. Lisa Littman had dared challenge one of the central tenets of trans activism, which is that a person’s gender identity is innate, like sexual orientation. Nobody, the activists insisted, could ever be persuaded into being trans.
The argument of many current trans activists is that if you don’t let a gender dysphoric teenager transition, they will kill themselves. In an article explaining why he resigned from the Tavistock (an NHS gender clinic in England) psychiatrist Marcus Evans stated that claims that children will kill themselves if not permitted to transition do not ‘align substantially with any robust data or studies in this area. Nor do they align with the cases I have encountered over decades as a psychotherapist.’
The writings of young trans men reveal a group of notably sensitive and clever people. The more of their accounts of gender dysphoria I’ve read, with their insightful descriptions of anxiety, dissociation, eating disorders, self-harm and self-hatred, the more I’ve wondered whether, if I’d been born 30 years later, I too might have tried to transition. The allure of escaping womanhood would have been huge. I struggled with severe OCD as a teenager. If I’d found community and sympathy online that I couldn’t find in my immediate environment, I believe I could have been persuaded to turn myself into the son my father had openly said he’d have preferred.
When I read about the theory of gender identity, I remember how mentally sexless I felt in youth. I remember Colette’s description of herself as a ‘mental hermaphrodite’ and Simone de Beauvoir’s words: ‘It is perfectly natural for the future woman to feel indignant at the limitations posed upon her by her sex. The real question is not why she should reject them: the problem is rather to understand why she accepts them.’
As I didn’t have a realistic possibility of becoming a man back in the 1980s, it had to be books and music that got me through both my mental health issues and the sexualised scrutiny and judgement that sets so many girls to war against their bodies in their teens. Fortunately for me, I found my own sense of otherness, and my ambivalence about being a woman, reflected in the work of female writers and musicians who reassured me that, in spite of everything a sexist world tries to throw at the female-bodied, it’s fine not to feel pink, frilly and compliant inside your own head; it’s OK to feel confused, dark, both sexual and non-sexual, unsure of what or who you are.
I want to be very clear here: I know transition will be a solution for some gender dysphoric people, although I’m also aware through extensive research that studies have consistently shown that between 60-90% of gender dysphoric teens will grow out of their dysphoria. Again and again I’ve been told to ‘just meet some trans people.’ I have: in addition to a few younger people, who were all adorable, I happen to know a self-described transsexual woman who’s older than I am and wonderful. Although she’s open about her past as a gay man, I’ve always found it hard to think of her as anything other than a woman, and I believe (and certainly hope) she’s completely happy to have transitioned. Being older, though, she went through a long and rigorous process of evaluation, psychotherapy and staged transformation. The current explosion of trans activism is urging a removal of almost all the robust systems through which candidates for sex reassignment were once required to pass. A man who intends to have no surgery and take no hormones may now secure himself a Gender Recognition Certificate and be a woman in the sight of the law. Many people aren’t aware of this.
We’re living through the most misogynistic period I’ve experienced. Back in the 80s, I imagined that my future daughters, should I have any, would have it far better than I ever did, but between the backlash against feminism and a porn-saturated online culture, I believe things have got significantly worse for girls. Never have I seen women denigrated and dehumanised to the extent they are now. From the leader of the free world’s long history of sexual assault accusations and his proud boast of ‘grabbing them by the pussy’, to the incel (‘involuntarily celibate’) movement that rages against women who won’t give them sex, to the trans activists who declare that TERFs need punching and re-educating, men across the political spectrum seem to agree: women are asking for trouble. Everywhere, women are being told to shut up and sit down, or else.
I’ve read all the arguments about femaleness not residing in the sexed body, and the assertions that biological women don’t have common experiences, and I find them, too, deeply misogynistic and regressive. It’s also clear that one of the objectives of denying the importance of sex is to erode what some seem to see as the cruelly segregationist idea of women having their own biological realities or – just as threatening – unifying realities that make them a cohesive political class. The hundreds of emails I’ve received in the last few days prove this erosion concerns many others just as much. It isn’t enough for women to be trans allies. Women must accept and admit that there is no material difference between trans women and themselves.
But, as many women have said before me, ‘woman’ is not a costume. ‘Woman’ is not an idea in a man’s head. ‘Woman’ is not a pink brain, a liking for Jimmy Choos or any of the other sexist ideas now somehow touted as progressive. Moreover, the ‘inclusive’ language that calls female people ‘menstruators’ and ‘people with vulvas’ strikes many women as dehumanising and demeaning. I understand why trans activists consider this language to be appropriate and kind, but for those of us who’ve had degrading slurs spat at us by violent men, it’s not neutral, it’s hostile and alienating.
Which brings me to the fifth reason I’m deeply concerned about the consequences of the current trans activism.
I’ve been in the public eye now for over twenty years and have never talked publicly about being a domestic abuse and sexual assault survivor. This isn’t because I’m ashamed those things happened to me, but because they’re traumatic to revisit and remember. I also feel protective of my daughter from my first marriage. I didn’t want to claim sole ownership of a story that belongs to her, too. However, a short while ago, I asked her how she’d feel if I were publicly honest about that part of my life, and she encouraged me to go ahead.
I’m mentioning these things now not in an attempt to garner sympathy, but out of solidarity with the huge numbers of women who have histories like mine, who’ve been slurred as bigots for having concerns around single-sex spaces.
I managed to escape my first violent marriage with some difficulty, but I’m now married to a truly good and principled man, safe and secure in ways I never in a million years expected to be. However, the scars left by violence and sexual assault don’t disappear, no matter how loved you are, and no matter how much money you’ve made. My perennial jumpiness is a family joke – and even I know it’s funny – but I pray my daughters never have the same reasons I do for hating sudden loud noises, or finding people behind me when I haven’t heard them approaching.
If you could come inside my head and understand what I feel when I read about a trans woman dying at the hands of a violent man, you’d find solidarity and kinship. I have a visceral sense of the terror in which those trans women will have spent their last seconds on earth, because I too have known moments of blind fear when I realised that the only thing keeping me alive was the shaky self-restraint of my attacker.
I believe the majority of trans-identified people not only pose zero threat to others, but are vulnerable for all the reasons I’ve outlined. Trans people need and deserve protection. Like women, they’re most likely to be killed by sexual partners. Trans women who work in the sex industry, particularly trans women of colour, are at particular risk. Like every other domestic abuse and sexual assault survivor I know, I feel nothing but empathy and solidarity with trans women who’ve been abused by men.
So I want trans women to be safe. At the same time, I do not want to make natal girls and women less safe. When you throw open the doors of bathrooms and changing rooms to any man who believes or feels he’s a woman – and, as I’ve said, gender confirmation certificates may now be granted without any need for surgery or hormones – then you open the door to any and all men who wish to come inside. That is the simple truth.
On Saturday morning, I read that the Scottish government is proceeding with its controversial gender recognition plans, which will in effect mean that all a man needs to ‘become a woman’ is to say he’s one. To use a very contemporary word, I was ‘triggered’. Ground down by the relentless attacks from trans activists on social media, when I was only there to give children feedback about pictures they’d drawn for my book under lockdown, I spent much of Saturday in a very dark place inside my head, as memories of a serious sexual assault I suffered in my twenties recurred on a loop. That assault happened at a time and in a space where I was vulnerable, and a man capitalised on an opportunity. I couldn’t shut out those memories and I was finding it hard to contain my anger and disappointment about the way I believe my government is playing fast and loose with womens and girls’ safety.
Late on Saturday evening, scrolling through children’s pictures before I went to bed, I forgot the first rule of Twitter – never, ever expect a nuanced conversation – and reacted to what I felt was degrading language about women. I spoke up about the importance of sex and have been paying the price ever since. I was transphobic, I was a cunt, a bitch, a TERF, I deserved cancelling, punching and death. You are Voldemort said one person, clearly feeling this was the only language I’d understand.
It would be so much easier to tweet the approved hashtags – because of course trans rights are human rights and of course trans lives matter – scoop up the woke cookies and bask in a virtue-signalling afterglow. There’s joy, relief and safety in conformity. As Simone de Beauvoir also wrote, “… without a doubt it is more comfortable to endure blind bondage than to work for one’s liberation; the dead, too, are better suited to the earth than the living.”
Huge numbers of women are justifiably terrified by the trans activists; I know this because so many have got in touch with me to tell their stories. They’re afraid of doxxing, of losing their jobs or their livelihoods, and of violence.
But endlessly unpleasant as its constant targeting of me has been, I refuse to bow down to a movement that I believe is doing demonstrable harm in seeking to erode ‘woman’ as a political and biological class and offering cover to predators like few before it. I stand alongside the brave women and men, gay, straight and trans, who’re standing up for freedom of speech and thought, and for the rights and safety of some of the most vulnerable in our society: young gay kids, fragile teenagers, and women who’re reliant on and wish to retain their single sex spaces. Polls show those women are in the vast majority, and exclude only those privileged or lucky enough never to have come up against male violence or sexual assault, and who’ve never troubled to educate themselves on how prevalent it is.
The one thing that gives me hope is that the women who can protest and organise, are doing so, and they have some truly decent men and trans people alongside them. Political parties seeking to appease the loudest voices in this debate are ignoring women’s concerns at their peril. In the UK, women are reaching out to each other across party lines, concerned about the erosion of their hard-won rights and widespread intimidation. None of the gender critical women I’ve talked to hates trans people; on the contrary. Many of them became interested in this issue in the first place out of concern for trans youth, and they’re hugely sympathetic towards trans adults who simply want to live their lives, but who’re facing a backlash for a brand of activism they don’t endorse. The supreme irony is that the attempt to silence women with the word ‘TERF’ may have pushed more young women towards radical feminism than the movement’s seen in decades.
The last thing I want to say is this. I haven’t written this essay in the hope that anybody will get out a violin for me, not even a teeny-weeny one. I’m extraordinarily fortunate; I’m a survivor, certainly not a victim. I’ve only mentioned my past because, like every other human being on this planet, I have a complex backstory, which shapes my fears, my interests and my opinions. I never forget that inner complexity when I’m creating a fictional character and I certainly never forget it when it comes to trans people.
All I’m asking – all I want – is for similar empathy, similar understanding, to be extended to the many millions of women whose sole crime is wanting their concerns to be heard without receiving threats and abuse.
All I’m asking – all I want – is for similar empathy, similar understanding, to be extended to the many millions of women whose sole crime is wanting their concerns to be heard without receiving threats and abuse.
Comment J.K Rowling has a problem with losing numbers of men to become more feminine mtf females. She shows approval of gay boys and men, implying that transsexuals are gays in denial. All of this is a fine demonstration of her fantasy writing skills. But we are not in the age of Hogwarts fantasy land.
The masses live in an increasingly brutal violent and conflicted society ( for want of a better world ) where Rowlings creatures and magic would not stand a chance. The monsters in the world of reality are more dangerous and unjust than than her creations. Her vile self centred genital obsessed attitudes to trans people are puting them at risk.
The absurd argument that trans women transition to molest women in rest and changing rooms, begs the question as to whether lesbians should be barred from female safe spaces. Equally , the idea that women never lie about rape or interfere with men, needs debunking and they should be kept out of male safe spaces
Having said that , I am no fan of the LGBTQI sheep pen which makes incumbents seem like frighetned sheep. I recall the age of April Ashley with whom I used to correspond , and Tula. Both became stunning Bond girls , merging comfortably into the female world.
The likes of Rowling, a lucky but not great writer, have an obsession with being women and raising doubts about whether all men are potentially violent. Fact is , women have at least as great a propensity to lying and violence but go about it in a different way. If they look glamorous they get away with it – as the media opined that Caroline Flack should. R.Jane Cook



https://unherd.com/2021/07/the-transgender-lobby-wants-to-rewrite-the-law/ From F.S July 8th 2021
| The Gen Z Conservative Newsletter Hi all, welcome back to the Gen Z Conservative newsletter! Today, we have six posts for you. Check them out below! If you would like to submit an article, meme, political cartoon, or any other content, just send an email to admin@genzconservative.com with your submission! I’d love to publish it. Read the guidelines here Enjoy reading and please forward this email to friends and family members who might be interested, as every share or forward helps! |
| Masculinity Isn’t Toxic. Ignore the Lies of the Tyranny-Minded Left |
| The greatest lie currently told by the modern left is that masculinity is toxic. That talking point, in various forms, has come from every segment of society. Teachers tell young boys not to fight, Gillette implies that flirting and grilling is toxic in its ads, school is designed to restrain energetic young men, and physical achievement is looked down upon … Read more |


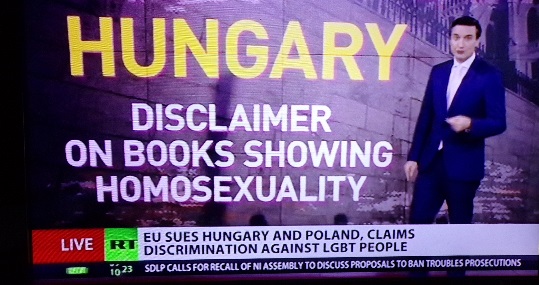
Stunning Evidence that the Left Has Won its War on White Males
July 15th 2021
There is a sickness in American society, fanned by the propaganda campaigns of the left, and it is killing people. White males, in large numbers, are simply losing their will to live, and as a result, they are dying so prematurely and in such large numbers that a startling demographic gap has emerged. It is not just the “opioid epidemic” that is killing off white working class males, it is a spiritual crisis, and Princeton economists Anne Case and Angus Deaton have the numbers to sustain this conclusion.
Jeff Guo of the Washington Post reveals the new findings of the two economists who first noticed the declining white male mortality.
The problem of dying whites can’t only be blamed on rising rates of drug overdoses, suicides and chronic alcoholism, they say. More and more, middle-aged white Americans are dying for all kinds of reasons — and the underlying issue may have less to do with opioids and more to do with how society has left behind the working class.
“Ultimately, we see our story as about the collapse of the white, high school educated, working class after its heyday in the 1970s, and the pathologies that accompany that decline,” they write.
This is slightly different than what they said in their first paper, where they emphasized that the trend of rising white mortality was “largely accounted for by increasing death rates from drug and alcohol poisonings, suicide, and chronic liver diseases and cirrhosis.” That’s technically correct — but by focusing only on the increase in death rates, Case and Deaton distracted from the larger picture.
The alarming fact isn’t just that middle-aged whites are dying faster, but also that mortality rates have been dramatically declining in nearly every other rich country. The United States is getting left behind.
That last point, that American white males are the exception, is the real proof that something particularly dangerous and harmful has been underway in American society. The two economists have summed up the relative change in mortality with this startling chart:
As Case and Deaton show, the gap in mortality between white middle-aged Americans and middle-aged Germans is about 125 deaths per 100,000 people now. Every year, of 100,000 Germans between the ages of 45 and 54, about 285 die. In the United States, it’s more than 410.
Out of those 125 additional American deaths, only about 40 might be explained by the spike in deadly drug use, drinking and suicides. And the rest? It’s hard to say. In their latest paper, Case and Deaton say that heart disease is part of the problem. While other countries have cut down heart disease deaths by over 40 percent in the past 15 years, heart disease remains a significant killer for white middle-aged Americans.

For at least four decades, white males have been under continuous assault as bearers of “white privilege” and beneficiaries of sexism. Special preferences and privileges have been granted to other groups, but that is the least of it. More importantly, the very basis of the psychological self-worth of white males have been under attack. White males are frequently instructed by authority figures in education and the media that they are responsible for most of the evils of the modern world, that the achievements of Euro-American civilization are a net loss for humanity, stained by exploitation, racism, unfairness, and every other collective evil the progressive mind can manufacture.
Some white males are relatively unscathed by the psychological warfare, but others are more vulnerable. Those who have educational, financial, or employment achievements that have rewarded their efforts may be able to keep going as productive members of society, their self-esteem resting on tangible fruits of their work and social position. But other white males, especially those who work with their hands and have been seeing job opportunities contract or disappear, have been losing the basis for a robust sense of self-worth as their job opportunities disappear.
We now have statistical evidence that political correctness kills.
A friend, David Kahn, comments:
This is terribly troubling. How all this has fallen outside the focus of our political debate is astonishing. This would seem to be at least as important as the issues of the day including which bathroom you can use, police abuse and who can be legally married to whom. It’s easy to understand why these people would resent the attention being paid to these issues and to the rights of the illegal immigrants.
There is a sickness in American society, fanned by the propaganda campaigns of the left, and it is killing people. White males, in large numbers, are simply losing their will to live, and as a result, they are dying so prematurely and in such large numbers that a startling demographic gap has emerged. It is not just the “opioid epidemic” that is killing off white working class males, it is a spiritual crisis, and Princeton economists Anne Case and Angus Deaton have the numbers to sustain this conclusion.
Jeff Guo of the Washington Post reveals the new findings of the two economists who first noticed the declining white male mortality.
The problem of dying whites can’t only be blamed on rising rates of drug overdoses, suicides and chronic alcoholism, they say. More and more, middle-aged white Americans are dying for all kinds of reasons — and the underlying issue may have less to do with opioids and more to do with how society has left behind the working class.
“Ultimately, we see our story as about the collapse of the white, high school educated, working class after its heyday in the 1970s, and the pathologies that accompany that decline,” they write.
This is slightly different than what they said in their first paper, where they emphasized that the trend of rising white mortality was “largely accounted for by increasing death rates from drug and alcohol poisonings, suicide, and chronic liver diseases and cirrhosis.” That’s technically correct — but by focusing only on the increase in death rates, Case and Deaton distracted from the larger picture.
The alarming fact isn’t just that middle-aged whites are dying faster, but also that mortality rates have been dramatically declining in nearly every other rich country. The United States is getting left behind.
That last point, that American white males are the exception, is the real proof that something particularly dangerous and harmful has been underway in American society. The two economists have summed up the relative change in mortality with this startling chart:
Read more: https://www.americanthinker.com/blog/2017/03/stunning_evidence_that_the_left_has_won_its_war_on_white_males_.html#ixzz70eJf2Yup
Follow us: @AmericanThinker on Twitter | AmericanThinker on Facebook
Comment I don’t think this matter is confined to the United State. It is certainly the case in the U.K. Sex change and other forms of feminisation are also outcomes , along with specific forms of self destructive crimes including the refuges of racism and misogyny.
You can’t have the white elite and BLM condemning whites , meaning working clas males , without consequences. Mental illness is another expanding issue. along with marriage collapse and white women taking sole charge of male offspring leading to behavioural issues. Robert Cook
Trans Ban – no room for transpeople in the Green Party – July 14th 2021
Berry, who was the party’s candidate for mayor, had been co-leader with Jonathan Bartley, who announced he was stepping down earlier this month. She said she had been agonising over whether to stand in the forthcoming leadership byelection but said she felt divisions in the party were too great.
A vocal supporter of trans equality, Berry had said one of the first things she would do as mayor would be to set up a commission on the rights of trans Londoners. In her resignation letter on Wednesday, Berry said there had been significant disagreement with colleagues elected to the party’s frontbench team. However, she did not give further details.
She said the party’s democratic structure meant decisions could be made that leaders did not agree with and she felt it was irreconcilable with her own position.
Sian Berry, is to quit as leader of the Greens, citing conflict within the party over transgender rights and claiming it had been a “failure of leadership” on her part that the party was sending “mixed messages”.
Train of Thought – R.J.C June 30th 2021

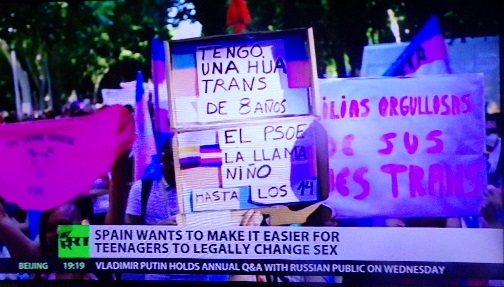
Feminist pressure groups are predominantly, if not entirely, upper middle class in origin and outlook. They insist on their ever extending rights , as a matter of birth entitlement. Females are , according to this mantra , an homogenous blob in all things that matter, only doing wrong when led astray by men , as with P.C Benjamin’s female sidekick.
So asking them to make any connections between anything that doesn’t fit their ‘we need more empowerment’ chant , is impossible. They subliminally claim that women will only use power for good , should have the right to do any job whilst claiming to be best suited to parenting. Responsibilities are not an issue for them because problems only occur where men obstruct their power. A female member of the House of Lords went as far as calling for a male curfew , following Sarah Everard’s rape and murder by an elite male Metropolitan Police officer.

So , we have a situation where women can dress as they please , as masculine as they like and claim occupancy of all former male safe spaces as means of protecting women from anything men might be plotting against their universal interest.

They work from the principle that all men are dangerous but BAME men have been equally oppressed as them , by white men. So it is quite right to berate all white men as privileged and white supremacists, If they are seen courting BAME women there is a new psychotic label for them. It is called fetishizing BAME women’s skin colour and nothing to do with ‘proper’ sexual attraction. The same rule does not apply to white women pursuing black men or to Prince Harry.
So against this background and in this context , it is not surprising that increasing numbers of young white males are seeking sex change at ever younger ages. This is not helped by the long standing marginalisation of white and black men from the nuclear family – the black response is less likely to lead to sex change because it is the white female who has made a fetish of herself , hence all the diverse clothing , make up , lingerie and shoes.
Young white boys have these usually self righteous patronising women as their nearest and most important role models. Feminists don’t like this truth because they refuse to accept nature while pathetically condemning transsexuals for going against the natural. They ally with Muslims who don’t understand this exploding western sex change phenomena because it goes against the God which is the basis of their culture , all pervading , putting and dressing women for their place.
So , on RT today we had a transwomen lawyer activist speaking up for the proposed law to make it easier for trans orientated young people to change sex. Feminists know that takers for this will be boys. Incredible numbers of girls have already adopted traditional male behaviour. It isn’t called sex change. That would be a hate crime. That is O.K for them because empowerment gives them the right to move freely and demand new laws always to make their lives happier and ‘safer.’ When they wear men’s clothes, shoes and haircuts they are expressing their rights. The only wrongs are firmly in the male camp and there is nothing worse for them than seeing a man wearing female clothes , shoes , perfume and make up.
Hence during today’s RT TV news clash between a trans woman lawyer and one of those very distinctive ‘female rights activists’ , the latter was not going to listen to the former. Her revulsion was palpable. Neither side , nor the interviewer posed the question why do so many pre pubescent children want sex change ? What is in their minds driving them to this extreme ?
Feminists don’t want to know because the answer might implicate them. Since the 1960s they have been on a self righteous roll. It started with more revealing clothes , in the knowledge of how easily deluded into romance men are. They expected to take over everything and emasculate men. They were the ones to decide what needed to change and how it would happen. Our elites have cottoned on to the use of the LGBTQI coral , but they also have to pander to feminists and Islamic vested interests.
I have written and read much on the subject of transgender. I am not making judgements here , beyond the foolishness of seeing sex change as solution to significant personal problems. The operatives in the system don’t care and are making it up as they go along.
In the U.K , the Gender Identity Clinic works on the principle that at least 90% of their sex change patients are mentally ill but wanting sex change is not a mental illness in its own right. I find that argument intriguing and extraordinary. I don’t wish to insult these people , but R.D Laing, a controversial psychiatrist from the 1960s, argued that State Psychiatrists ( of which he was one ) were whores to the system and its goals.
Explain to me why a mentally ill patient would be trusted with other peoples’ lives ? Then explain why a mentally ill person would be trusted to agree to a life changing series of interviews , with a psychiatrist, to explain why they should have gender re assignment treatment and surgery. Explain how their self assessment and the psychiatrists could safely conclude anything in these circumstances and then recommend mind numbing anti psychotic drugs to help the process along.
Either the system and its so called experts are utterly insane , or there is a hidden agenda. I am not siding with bigoted trans exclusionary feminists who are clearly obsessed with the sanctity and purity of their CIS gender and agenda. By law they are committing hate crime. I am just asking logical questions .
I know how the NHS GIC process works in Britain and where the Spanish experiment is heading. In the U,K they don’t ask patients why they don’t want to be men. They don’t even discuss what the patient might think gender is. How could a pre pubescent boy in a one parent family sensibly know the answer to that ? Hectoring feminists can only make life worse for trans girls. Feminists seem to believe , with media encouragement, that hate crimes only work one way.
The system is not honest , as we see with health service boss Hancock , and State goals are about what is expedient for the elite. At this moment in time , male sex change involves effective castration along with a cocktail of drugs which often involve anti psychotics. The whole process is not a picture of innocence or well meaning. Trans exclusive radical feminists are all about themselves. They want criticism of women , including them , made a hate crime. They don’t see or accept that their attitude to trans girls ( they are not worried about girls becoming boys ) is serious hate crime , so they don’t have the right to free speech on the matter. They get away with the most appalling statements, including saying that men have sex change treatment to hide away in female toilets to commit sex crime. This double standard is almost black comedy – no racist meaning intended.
This army of hectoring women do not however , accept that their blanket attitude and condemnation of trans people is a hate crime. These people only shout for laws that protect them and do not care if they harm others. They are just as obsessed with gender as the transsexuals they condemn. Their attitude to men does inspire hate and they are thus only looking after themselves and their growing power. Their arguments do not have to be consistent. They are to be taken as truth. Robert Cook
Train company praised for ‘incredible’ response following complaints over rainbow-coloured Pride train(sexual).
June 28th 2021

A Scottish rail company’s response to a customer questioning the need for their rainbow-coloured Pride train has gone viral on social media.
ScotRail was praised for its blunt answer after a Twitter user asked the firm if they would also be painting a train in “straight colours,” adding: “Or will we be discriminated against?”
But a no-nonsense social media manager went viral, after replying: “Straight people aren’t punched in the face for holding hands with their life partner, nor are they executed in other countries simply for being straight.
Maya Forstater’s transgender views should be ‘tolerated in society’, judge rules Posted June 10th 2021
By Josh Payne, PA 1 hour ago National Geographic recognizes new Southern Ocean, bringing global… Saweetie: I won’t compromise my morals
The views of a woman who lost her job after claiming people cannot change their biological sex should be “tolerated in a pluralist society”, a High Court judge has ruled.
Maya Forstater’s contract was not renewed in March 2019 after she posted tweets opposing government proposals to reform the Gender Recognition Act to allow people to identify as the opposite sex.
On Thursday, Ms Forstater, who worked as a tax expert at the Centre for Global Development (CGD), won her appeal against an employment tribunal, a judgment which the international think tank described as “a step backwards for inclusivity and equality for all”.
Mr Justice Choudhury said the original tribunal had “erred in law”, but added: “This judgment does not mean that those with gender-critical beliefs can ‘misgender’ trans persons with impunity.”
Finding in favour of Ms Forstater, the High Court judge said her views “may well be profoundly offensive and even distressing”, but said they “must be tolerated in a pluralist society”.
Mr Justice Choudhury acknowledged “some trans persons will be disappointed by this judgment”.
Ms Forstater originally took her case to an employment tribunal on the grounds that her dismissal constituted discrimination against her beliefs.
But employment judge James Tayler previously dismissed her claim, saying her views are “absolutist in her view of sex”.
During the employment appeal tribunal in April, she reiterated her views that biological sex is “real, important, immutable, and not to be conflated with gender identity”.
Harry Potter author JK Rowling previously came out in support of the claimant, tweeting: “Live your best life in peace and security.
“But force women out of their jobs for stating that sex is real?”
In the judgment handed down on Thursday, Mr Justice Choudhury said: “We do not in any way seek to ignore or downplay the difficulties faced by trans persons seeking merely to live their lives peacefully in the gender with which they identify, irrespective of their natal sex.
“The regrettable reality for many trans persons, however, is that something which most take for granted – the sense of self and autonomy in identity – is under constant challenge and attack.
“This case, however, is not about whether greater protection ought to be afforded to trans persons.
“This appeal is about the much narrower issue of whether the claimant’s belief as to the immutability of sex is one that amounts to a philosophical belief under section 10 of the Equality Act 2010.
“We have come to the conclusion that it does.”
The High Court judge continued: “The claimant’s belief might well be considered offensive and abhorrent to some, but the accepted evidence before the Tribunal was that she believed that it is not ‘incompatible to recognise that human beings cannot change sex whilst also protecting the human rights of people who identify as transgender’.
“That is not, on any view, a statement of a belief that seeks to destroy the rights of trans persons.
“It is a belief that might in some circumstances cause offence to trans persons, but the potential for offence cannot be a reason to exclude a belief from protection altogether.”
Commenting on the judgment, executive vice president of CGD Amanda Glassman said: “The decision is disappointing and surprising because we believe Judge Tayler got it right when he found this type of offensive speech causes harm to trans people, and therefore could not be protected under the Equality Act.
“Today’s decision is a step backwards for inclusivity and equality for all.
“We’re currently considering the various paths forward with our lawyers.”
Also reacting to the ruling, Baroness Kishwer Falkner, chair of the Equality and Human Rights Commission, said: “Some may see the beliefs of others as questionable or controversial, but people must be free to hold them.
“This is why this case is so important.
“It provides clarity that people are free to hold their beliefs and must not be discriminated against because of them even if others might find their beliefs offensive.
“There is a difference between holding a belief and how it is expressed.
“We are all responsible for what we say and do.”
Comment Women like Maya Forstater are the driving force behind intolerant mind destroying political correctness so it is too bad when it turns around and bites them. Why should her kind have freedom of speech when so many of us do not.
The most notable thing about modern women and transsexuals is their obsession with female gender. It is very interesting and most significant in these peculiar and dangerous times. The two groups appear to be in serious competition on the matter. It is almost funny. But why has being female become so important and contentious ? What does empowerment mean ?
What does it mean to be female. Why does the London Gender Identity Clinic ask patients why they want to be women rather than why they don’t want to be men ? Why don’t they ask them what they think being a man or woman involves or how it is defined these days.? Why don’t they ask about how having babies links to that definition – in this era of falling white birth rates and stark career empowerment obsession ?
It seems the right to free speech is highly selective, favouring PC women. Why is it O.K to label men as suffering from ‘toxic masculinity and a proclivity toward ‘mansplaining’ ?
There appears to be no official effort to explain why so many boys and men want to appear as the opposite sex. My book ‘Man, Maid, Woman’ offers a very unacceptable explanation based on logic. Women’s groups and their slavish minions of both genders do not want to take responsibility , only to declaim against transsexuals. The one parent family link is heresy against feminism.
Robert Cook

This man fought for his country in two armed services. It is such a privilege being a white man in today’s inclusive diverse society.
Image by Robert Cook / Appledene Photographics August 2020.
Trans female MMA fighter lashes out at Joe Rogan, says he should stop talking about transgender athletes – Posted June 9th 2021
A transgender female athlete said that Joe Rogan should stop talking about the contentious issue of transgender people competing in sports. Fearless with Jason Whitlock
Fallon Fox retired from fighting professionally in 2014, but regularly speaks out in defense of transgender athletes. Fox was born a biological male.
The 45-year-old spoke out against Rogan and other critics of transgender athletes in an interview with ET Canada.
“A lot of prominent people were talking about a bunch of horrible things. The Joe Rogans, the Ronda Rouseys, the Dana Whites of the world,” said Fox.
“From what they said about me in the past, I could have just crawled up into a ball and given up. I could have just stopped competing, but I didn’t,” Fox explained. “I kept competing and I kept talking about this issue and I’m going to continue to do it.”
Fox went on to opine that Rogan, one of the most successful podcasters in history, should simply stop talking about transgender athletes.
“No, he shouldn’t speak, especially on this issue that’s so important to transgender people and transgender people’s lives,” Fox asserted. “Just like coronavirus is important to people’s lives. He just brings up these things and just makes them up.”
Fox argued against Rogan’s claim that biological males had an advantage over women because of their natural bone density differences.
“African-American women have more dense bones than Caucasian women do. I don’t see any one saying that we shouldn’t have African-American women competing against cisgender women,” Fox explained.
“I think it’s just bogus for them to even bring up bone density in the first place,” Fox concluded. “Things like that that people just bring out of thin air and just say our true, that [is what] we’re fighting against.”
Fox went on to complain that Rogan and others like him don’t appreciate her importance to the world of sports.
Rogan has been criticized by many on the left for arguing against the practice of hormone therapy for young children who may exhibit some gender confusion.
“There’s no reason to give kids hormones,” said Rogan on his podcast in 2019.
“People don’t know who they are, a 7-year-old,” he continued, “people don’t even give their 7 year-old phones, you don’t let them vote, you’re gonna let them decide what sex they’re gonna be for the rest of their life?”
‘We are still the unseen’: The horrific discrimination faced by transgender people of colour Posted June 1st 2021
Josh Marcus 47 mins ago James Knappett: The Michelin-starred chef bringing the art of… James Bond fears Amazon’s MGM buyout means tech giant may meddle 
On 14 June, during a summer of expansive nationwide protests against police brutality in the wake of George Floyd’s murder, an estimated 15,000 people gathered in Brooklyn, New York, for pride-month-converged”>Brooklyn Liberation, a rally for Black trans lives.
It’s believed to be the largest ever gathering of its kind, and it was a reminder about the many ways the fight for Black and trans justice are bound together historically, particularly when it comes to pushing back against police violence. One of the first people killed by police after Mr Floyd was Tony McDade, a 38-year-old Black transgender man, in Florida.
Now, a year on from George Floyd’s murder, activists and organisers say there’s a new energy around making the criminal justice system a more just place for trans people.
Still, they warn there’s a long way to go before trans lives, subject to both universal and extremely specific forms of discrimination and violence, truly matter to police and society at large.
The current criminal justice landscape for trans people is dire. They’re nearly four times more likely to experience police violence than cisgender people, while more than 20 per cent of Black trans women will be incarcerated at one point their life, a percentage far higher than that of the general population.
As of 2019, only 10 of the 25 biggest police departments included gender identity language in their non-discrimination policies, according to the National Center for Transgender Equality (NCTE). More than half of trans people the NCTE surveyed said they were harassed or abused when they interacted with law enforcement, and more than half also reported they feel uncomfortable calling the police for help. This fear of law enforcement persists, even as, broadly speaking, 2020 was the deadliest year ever for trans people, with more than 30 being murdered, especially trans women of colour.
As with most societal problems, anti-trans police violence becomes particularly acute against people of colour, who face all the stereotypes and biases any other person of colour would in addition to anti-trans bias.
“Transgender people of colour are much more likely to face this kind of harassment and outright violence from white police officers than other people,” Rodrigo Heng-Lehtinen of the NCTE told The Independent. “They’re much more likely to be stopped. They’re much more likely, especially Black trans women, are so much likely to be suspected of doing sex work.”
Sex work, in particular, is the axis on which huge amounts of police violence towards trans people turns. Because of pervasive interpersonal, housing, and employment discrimination, many trans people do engage in sex work to survive—more than 10 per cent, according to the US Transgender Survey—yet police often stop trans people on the assumption they’re all engaged in sex work. Meanwhile, laws in numerous states, frequently abused to target trans people, allow police to bring criminal charges against people carrying too many condoms, even though regular condom use is a key way to combat the HIV/AIDS epidemic, which also disproportionately affects trans people.
“Most people do not realise the pervasive issue of sexual assault by police officers that is way higher for trans women, especially Black and Latinx women, we hear horror stories of coerced sex, where police officers stop a trans person and say, ‘Give me what I want and I won’t arrest you,’” Mr Heng-Lehtinen said. “The other word for that is sexual assault.”
In some states, particularly in the South, trans people suspected of being sex workers can be hit with charges of “crimes against nature”, condemning them to life on the sex offender list even if they engaged in a consensual encounter.
This set of conditions – a formal economy where trans people are unwanted, and a legal system that punishes them for finding work in the informal or black market world – creates an impossible cycle of recidivism for many trans people in the justice system.
“You’re put in the revolving door of the prison-industrial complex. Then you have even more limited options when it comes to surviving,” said Aria Sa’id, a former sex worker and co-founder of San Francisco’s Transgender District neighbourhood, the world’s first legally recognised trans district. “After you’ve been incarcerated for a certain number of times, you’re no longer able to access traditional forms of employment. No one hires you. No one wants you to live in their neighbourhood.”
The problems aren’t limited to street-level contact with police, though; they’re built into the broader criminal justice system itself. Police reports frequently misgender and “dead name” trans people, while police in many jurisdictions are allowed to strip-search trans people to determine their gender. Some states even recognise a “trans panic defence”, a justification that uses one’s shock or emotion at finding out that someone is trans to explain violence against them.
Perhaps most pressing, according to trans justice advocates, is what happens inside of prisons. Trans people are frequently misgendered, or put in solitary confinement to protect them from other inmates.
“Roughly four in 10 incarcerated Black trans people have been sexually abused,” according to Scott Greenberg, from the LGBTQ Freedom Fund, a bail fund and advocacy group. “That’s as often by guards as other inmates, which is extraordinarily high.”
As a result of the deep interrelation between societal discrimination, race, policing, and sexuality – it is only a recent reform that being gay or even cross-dressing is not explicitly illegal – the histories of the trans civil rights movement and anti-police brutality work are frequently related, if not simultaneous. After police violently raided New York City’s Stonewall Inn, a popular gay gathering place, in 1969, trans and nonbinary people of colour led protests and riots against police brutality, as well as the first Pride march a year later.
Part of the impetus behind establishing San Francisco’s trans district was to preserve the history of the Compton’s Cafeteria Riots of 1966, one of the first recorded transgender riots in history, in response to frequent police mistreatment in the Tenderloin neighbourhood, known then as the city’s “gay ghetto”.
Carrying on that legacy, two of the three Black Lives Matter founders identify as queer, and numerous leaders in racial justice protests across the US after George Floyd’s murder were LGBT+ people of colour.
After centuries of Americans being totally unaware of or outright hostile to trans people, and decades of LGBT+ criminal justice issues being relegated to the sidelines of larger civil rights movements, Mr Floyd’s murder may have finally made the mainstream culture see the intersectional nature of these issues, according to activists.
“I think the murder of George Floyd in particular gave activists, with the support of the broader public, we were able to push policy pieces and initiatives that I just don’t think would’ve been successful five to 10 years ago, when we were seeing the murders of Trayvon Martin and Mike Brown. The broader American public did not want to have that nuanced understanding,” Ms Said, from San Francisco’s Trans District, said, pointing to initiatives like the city’s emergency Covid funds directed to LGBT+ people , which passed well before national stimulus cheques arrived.
“It’s unfortunate that so many people have had to be murdered in that way for more people to understand.”
Still, despite renewed national vigour around civil rights organisers, there has been an equally potent campaign against trans people in the same institutions they’re trying to reform. Across the country, Republican legislatures have introduced numerous bills aiming to prevent trans people and children from fully accessing healthcare, sports, and other areas.
“I’m speaking to you from a red state,” said Collette Carter, interim director of Breakout, a group working to end “the criminalisation of LGBTQ youth” in New Orleans, Louisiana, a state considering a host of anti-trans bills this legislative session. “I wish there was a better understanding, especially when it comes to LGBTQ Black people and communities of colour. We are still the unseen.”
During George Floyd protests last summer, Ms Carter says local police still tear gassed and mass-arrested overwhelmingly peaceful LGBT+ protesters, even though New Orleans has been under federal supervision for its police practices since a 2012 consent decree with the Department of Justice.
“Our folks were teargassed, physically engaged with with the police,” she said. “There wasn’t a broken window. Not a Target scratched. Not for the level of teargas and bulls*** they were pulling, in a consent decree city.”
Stopping this sort of discrimination requires drastic changes to culture, housing, employment, and policing all at once, experts say, since they all combine to yield the untenable present for trans people.
“At the end of the day, as long as there are high levels of discrimination across all these different areas of society, as long as families are discriminating against trans people, as long as they’re going to be discriminated in employment, you’re going to see high representation of trans people in the criminal legal system,” Greenberg, from the LGBTQ Freedom Fund, said. “The structural effects of marginalisation aren’t going to be dramatically changed by people in power passing a piece of legislation.”
But these challenges haven’t stopped LGBT+ organisers from pushing for a world where trans people are safe from police violence and discrimination in the criminal justice system.
“We’re here,” Ms Carter said, “We’re proud. And we’re fighting.”
Just like they always have been.
Transgender woman weightlifter Laurel Hubbard in Olympics is ‘like a bad joke’ to biological female athletes, competitor complains Posted June 1st 2021
NewsDave Urbanski May 31, 2021 Photo by Alex Pantling/Getty Images Like Blaze News? Get the news that matters most delivered directly to your inbox.SIGN UP
Transgender woman weightlifter Laurel Hubbard competing in the upcoming Tokyo Olympic Games is “like a bad joke” to biological female athletes, a rival weightlifter told Inside the Games. POLL: What scares you the most?
What are the details?
“First off, I would like to stress that I fully support the transgender community, and that what I’m about to say doesn’t come from a place of rejection of this athlete’s identity,” weightlifter Anna Van Bellinghen of Belgium told the sports website.
But she soon added that “anyone that has trained weightlifting at a high level knows this to be true in their bones: this particular situation is unfair to the sport and to the athletes,” Inside the Games said.
Van Bellinghen, 27, is looking to qualify in the same weight category as New Zealand’s Hubbard — the over-87-kilogram super-heavyweights — and is directly affected by the presence of Hubbard, who’s set to become the first openly transgender athlete to qualify for the Olympics in any sport, the website reported.
Hubbard, 43 — a biological male who identifies as female and has competed against women for several years — began transitioning to female at age 35.
It would seem Van Bellinghen’s complaints about Hubbard go against the wishes of the powers that be, who allegedly want those who disagree with Hubbard’s presence to be quiet about their concerns — but she went for the jugular anyway.
Van Bellinghen pointed out to Inside the Games that it’s widely known athletes can retain the benefit of taking steroids even years earlier — so therefore “why is it still a question whether two decades, from puberty to the age of 35, with the hormonal system of a man also would give an advantage [in competing against women]? I understand that for sports authorities nothing is as simple as following your common sense, and that there are a lot of impracticalities when studying such a rare phenomenon, but for athletes the whole thing feels like a bad joke.”
She added to the sports website that Hubbard’s presence means “life-changing opportunities are missed for some athletes — medals and Olympic qualifications — and we are powerless. Of course, this debate is taking place in a broader context of discrimination against transgender people, and that is why the question is never free of ideology. However, the extreme nature of this particular situation really demonstrates the need to set up a stricter legal framework for transgender inclusion in sports, and especially elite sports. Because I do believe that everyone should have access to sports, but not at the expense of others.”
Anything else?
Hubbard made a splash in 2017 after winning two silver medals in a women’s world championship — and then in 2019 took home two gold medals and a silver medal in the women’s competition at the Pacific Games in Samoa.
In 2015, IOC guidelines ruled that transgender athletes can compete as women if their testosterone levels are below 10 nanomoles per liter for at least 12 months before their first competition, Reuters reported.
But numerous scientists have criticized these guidelines, saying they do little to mitigate the biological advantages of those who have gone through puberty as males, including bone and muscle density, Australia’s 7 News reported.
Comment Cutting to the chase, sport is about money and ego. It is also about power and skill , dependent on muscle mass. This controversy gives the lie to female equality. Testosterone builds muscle and males have more of it.
Testosterone also accounts for other differences, significantly in temperament and spatial skill. If feminists really believe in equality , then they should shut up about this ludicrous issue of transwomen in female sport. The equality movement is all about power among the masses , with women campaigning for ever more laws to disadvantage and scapegoat white men. They want men to change, so some men go to the extreme and women don’t like it.
The alacrity with which feminism has embraced BAME and BLM is welcomed by the elite who do not want their real bastion of power challenged – that included not sorting out real inequality in Africa and India. Women’s groups only talk about themselves and the female blob. They demand laws to control speech, already having made serious gains and attacks on male identity – with little boys queuing up to change sex. They really don’t like men stealing their clothes. It is very funny.
It also means encouraging religious bigotry and divisions as a distraction from poverty and tyranny , blaming everything on white working class masses throughout history , even though only a black and white elite made gain from slavery while enslaving their own , is the trick. Modern sport is an obscene money machine which transwomen want to cash in on.
Robert Cook
British theatres pledge to only cast transgender actors in trans roles Posted May 26th 2021
Milly Vincent For Mailonline 2 hrs ago Man sees house collapse just yards from him and barely breaks stride Sylvester Stallone sports all-black at Craig’s in LA with his family 
A group of British theatres says it will only cast transgender actors in trans roles, joining a heated debate over whether performers must mirror the sexuality or gender identity of LGBT+ characters they play on stage or screen.
The ‘Trans Casting Statement’, signed by over 40 theatres and production companies – including London‘s prestigious Royal Court and the Oxford Playhouse – also committed to ‘actively seek casting opportunities’ of any gender for trans actors. Advertisement
In a statement, the theatres said their aim was to boost trans visibility on stage and better support what can be a marginalised community.
Hollywood actors who are not trans have won Oscars for playing trans characters, including Jared Leto for ‘Dallas Buyers Club’ in 2014.
But in recent years Halle Berry and Scarlett Johansson have pulled out of roles after criticism.
‘This statement is hugely necessary,’ Reece Lyons, a trans actor said.
‘Trans people are a hugely marginalised community. We’re facing a lot … of negative media and press attention.
‘If a role is a trans-specific role, then the actor who takes on that role needs to have the lived experience to be able to portray the nuance of that experience,’ she said.
The view that only LGBT+ actors should play LGBT+ characters has been criticised by some in the industry who say that roles should be available to the best actor for the part.
Similar disputes have erupted over who should perform disabled and Black roles on stage or the merits of women performing male parts in Shakespeare.
‘I would certainly audition for a trans role if I felt it was a role I wanted to play in a production I liked,’ Sam Lockley, a non-transgender actor and writer, said by email.
‘I would also audition for a role whose sexuality I don’t share, or whose political views I don’t share. It’s part of acting to play people that are different from you.’
Scarlett Johansson, a cisgendered actress, dropped out of playing a transgender character in the movie Rub & Tug in 2019, apologising for having been ‘tone-deaf’ to criticism.
Johansson told Vanity Fair at the time: ‘I mishandled that situation.
‘To feel like you’re kind of tone-deaf to something is not a good feeling.’
Female student, 29, who said ‘women have vaginas’ and are ‘not as strong as men’ faces disciplinary action by university after fellow classmates complained about the ‘offensive and discriminatory’ comments – May 18th 2021
- Lisa Keogh facing disciplinary action at Abertay University in Dundee, Scotland
- The student said women were born with female genitals during a video seminar
- She was reported to university’s chiefs by her classmates following the debate
By Bhvishya Patel For Mailonline
Published: 02:03, 15 May 2021 | Updated: 17:43, 15 May 2021
A student who said women were born with female genitals and the difference in physical strength between men and women ‘was a fact’ is facing disciplinary action by her university.
Lisa Keogh, 29, who studies law at Abertay University in Dundee was reported to university chiefs by her classmates after she said that women were not as physically strong as men.
The mature student, who is in her final year, is now facing a formal investigation by the university for the alleged ‘offensive’ and ‘discriminatory’ comments.
The mother-of-two said she had been taking part in a video seminar about gender feminism and the law when she raised concerns about trans women taking part in mixed martial arts.
- Following the debate, in which Ms Keogh claims she was muted by her lecturer, the mature student was met with a flurry of abuse from her fellow classmates. Pictured, Abertay University in Dundee
After telling her classmates that a women who had testosterone in her body for 32 years would be genetically stronger than the average woman, the mature student was accused of calling women the ‘weaker sex’.
She told The Times: ‘I thought it was a joke. I thought there was no way that the university would pursue me for utilising my legal right to freedom of speech.’
Following the debate, in which Ms Keogh claims she was muted by her lecturer, the mature student was met with a flurry of abuse from her fellow classmates.
Ms Keogh, who is being supported by Joanna Cherry QC, the SNP MP for Edinburgh South West, continued: ‘I didn’t intend to be offensive but I did take part in a debate and outlined my sincerely held views.’
She added: ‘I wasn’t being mean, transphobic or offensive. I was stating a basic biological fact.’
Comment Though I agree with this female student, there is an irony. Feminists are always telling us that women are equal . The sexes – or must I say genders – are not equal , people are not equal. The basic equality issue is money. The rest is a smokescreen.
Physically men and women , on average are not equal. Females cannot match men in any sport where power , spatial awareness and stamina are the issue. Twisting and limiting language, which is the woke norm , to argue that TS women are or are not biological women will not alter reality.
Female ‘sports ‘ stars are worried about their egos and the money and they should because any male who has transitioned after puberty will beat them. They don’t like being told that , but they don’t like the competition either.
There is also the more disturbing truth that this mature female student was shut up by her lecturer , abused and now faces disciplinary action. All the signs are that Britain is an advanced police state. That is why the authorities and their media keep telling us it is a democracy. LGBTQI is a prison , lifestyle choice at best.
Peoples’ sex lives , like their religion should be private matters. But the elite need to make issues of all of this. This mentality doesn’t stop here. It is Nazism. Stifling this girl’s statement of the obvious is just another example that anyone caught saying or writing the wrong thing will face judgement by the vurtue signallers and punishment by the British Police State.
Robert Cook.
Mayflower & The New New World by Robert Cook May 12th 2021
I took the above photo as one of a series while working on a book called ‘Southampton Past & Present.’ It was the inspiration for my subsequent novel in the same year, 2003 , ‘Man , Maid, Woman.’
The ‘Mayflower’ called at Southampton on its way from London and then to Plymouth before crossing the Atlantic with its cargo of Puritans , founding ‘The New World’ in 1620.
Finding new worlds now is pretty well impossible with so many people, greedy elites and competing cultures. Here we have an alternative Mayflower New World as transvestites and transsexuals come out in growing numbers.
Such people provoke extreme reactions. London’s Gender Identity Clinic take the view that transsexualism is not mental illness, but most of their patients have other mental illness which a sex change process can do a lot to help. Stringent anti hate laws make a critical examination of these sensitive matters.
I will , however, return to this subject as and when I see fit , because it is a fundamental socio psychological condition. Why it exists and how it should be treated are two of the key questions , along with why and how it appears to manifest itself and to be encouraged from ever younger pre puberty ages. Robert Cook
Alabama Enacts Law Banning Transgender Athletes From Participating in Biologically Inconsistent Public School Sports Posted April 28th 2021
Alabama Gov. Kay Ivey has signed into law a bill that bans transgender student-athletes from competing on K–12 public school single-sex teams that match their gender identity.
House Bill 391, which was overwhelmingly approved by the Republican-controlled state legislature last week, mandates that those who aren’t biologically male or female won’t be able to participate in school-sponsored sports events that are inconsistent with their sex assigned at birth.
“A public K-12 school may not allow a biological female to participate on a male team if there is a female team in a sport,” the bill reads. “A public K-12 school may never allow a biological male to participate on a female team.”
According to the bill, it’s important to make sure sports teams remain separate and sex-specific so that female athletes can have equal opportunity to compete, considering inherent athletic advantages for biological males including, on average, a larger body size, more skeletal muscle mass, lower percentage of body fat, and greater maximal delivery of anaerobic and aerobic energy.
The bill doesn’t specify how student-athletes can prove their biological sex, although its earlier version said that will be determined by their birth certificates.
Already this year, Arkansas, South Dakota, Mississippi, and Tennessee also joined Idaho’s 2020 ban on transgender athletes in school sports, which was later blocked by a federal judge and is currently pending legal review. Tennessee was the first U.S. state to ban both transgender girls and boys from participating in corresponding single-sex school sports, while all others only ban transgender girls. South Dakota’s ban was enacted by executive order, not by legislation.
The states’ legislative efforts came as the Biden administration pushed to open up single-sex spaces and competitions to members of the opposite sex, depending on the person’s stated gender identity. An executive order signed by President Joe Biden on his first day in the White House states that it’s the new administration’s policy to make sure children are able to “learn without worrying about whether they will be denied access to the restroom, the locker room, or school sports.”
Miguel Cardona, who was confirmed in March as the new U.S. secretary of education, also said during his Senate confirmation hearing that he believes it’s the right of male-born transgender students to compete in girls’ sports.
“I think it’s critically important to respect the rights of all students, including students who are transgender, and that they are afforded the opportunities that every other student has to participate in extracurricular actives,” Cardona said at the time.
I don’t know what I think about the reality of female brains in male bodies. The reality that feminism offers and encourages females into a more aggressive male type behaviour, dressing accordingly seems to pass unnoticed by media et al. After all , this is the age of equality ( sic )
But when boys want to be like girls , girls are upset and the equality loving feminists play the SIS gender card. They fear unfair competition and rape from people they still regard as men , but without penises.
Depending on how one looks at this , it is either laughable or sad. Fathers pushed out of homes on dubious grounds that must not be talked about because women are always right and truthful must not be mentioned . Girls like BAME have rights to positive role models , but that is not so for little white boys. As for little black boys , unless they have rich parents , gang crime is a favoured way of finding their sense of identity and belonging.
It isn’t good. One suspects , knowing Alabama , religion has something to do with this righteous ban. R.J Cook
Typical Woman – she just can’t make up her mind. Posted April 18th 2021
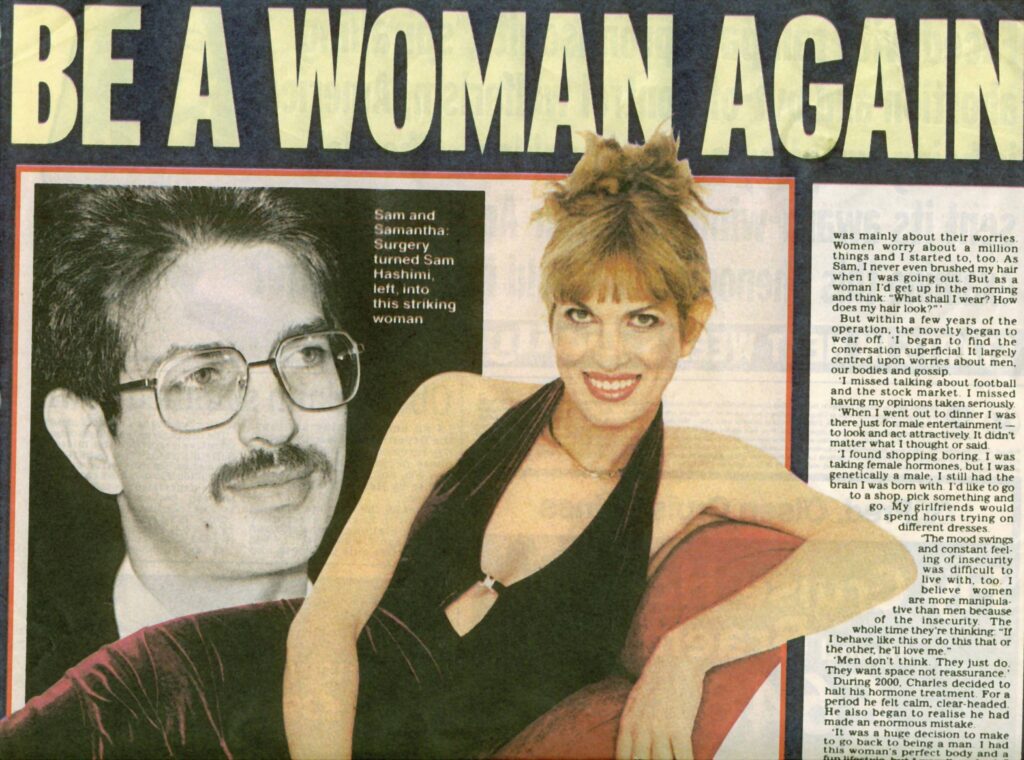
More to come on this interesting case.
A high-flying transgender lawyer has revealed how she has undergone a gender re-assignment operation for the third time – after going back to being a man in a bid to reconnect with her children.
Samantha Kane, from west London, explained how she felt she ‘had no choice’ but to transition back to a woman again, following two previous sex changes, and now feels like her ‘true self’ again.
The lawyer and author, who was born Sam Hashimi in Baghdad, Iraq, first underwent gender reassignment surgery back in 1997, becoming Samantha.
But in 2004, she decided she wanted to go back to being a man, undergoing another operation to become Charles, having become estranged from her son and daughter following her first sex change.
Earlier this year, Samantha, 58, underwent surgery to become a woman again, spending a total of over £150,000 on gender re-assignment operations over the years.
Speaking to FEMAIL, Samantha admitted that her decision to transition back to a man had been largely influenced by a desire to see her children, who she became estranged from after divorcing first wife Trudi in the early 1990s.
‘I couldn’t see my children for around 10 years, I started missing them so much,’ she explained. ‘My children grew up not really knowing me. It was so difficult.
‘Eventually, I thought, maybe I could get back what I love if I changed back, and became a man again. That’s really the reason [I did it].’
However, Samantha said that within a year of living as a Charles, she began to realise that she had made a mistake in transitioning back to a man – particularly as the gender reassignment surgery hadn’t gone as expected.  +8
+8
Samantha had been living as Charles Kane (above, pictured at home in London in 2008) since 2004. She explained how she had decided to go back to being a man in a bid to re-connect with her children, who she became estranged from after becoming Samantha for the first time
‘In the first year, I had regrets – what they claimed the operation would achieve, they never achieved anyway,’ she said.
‘Turning a man who was born a man into a woman, and then approximating back to what it was like being a male will never work – that was really part of it.’
At the time, Charles was engaged to a woman named Victoria, but the relationship quickly broke down.
‘I was feeling uncomfortable. I was in a relationship with a woman and it was expected of me to be all male really,’ Samantha explained.
‘As Charles, I wasn’t 100 per cent accepted. I was having these regrets of changing back.’  +8
+8
Samantha underwent her first sex change in 1997, when she went from being Sam to Samantha. She is pictured here in Monaco in 2001
A timeline of Samantha’s journey
1960 – Born a man, Sam Hashimi, in Baghdad, Iraq
1997 – Transitioned to a woman, living as Samantha Kane
2004 – Underwent second gender re-assignment surgery to go back to being a man, and began living as Charles Kane
2017 – Began living as Samantha again
2018 – Underwent third gender re-assignment surgery to complete transition Advertisement
However, Samantha explained how she didn’t want to transition back to a woman straight away – in part, due to her high-flying career as a barrister.
‘I went through all this trouble to be Charles, and one had to make the best out of it I suppose,’ she said.
‘I’m a lawyer, and thought people wouldn’t understand me changing back. At the Bar, people have to adopt more tradition roles. Chopping and changing is frowned on.’
But Samantha explained how re-connecting with her adult son eventually helped her decide to transition back to a woman.
‘I saw him shortly before his wedding, and he told me he was getting married, and he invited to me to his wedding. That was really nice,’ she said.
‘He said, “I don’t mind who you are. I love you whether you are a male or a female. If it makes you be happier to be a female, then so be it.”
‘That’s what encouraged me to change back basically. He’s very supportive.’
Samantha began dressing as a woman in March last year, and airier this year had gender re-assignment surgery and breast implants fitted.
The lawyer says that since the operation in January she now finally feels like herself again, after all these years.
‘I feel a lot better in myself now. I came to the conclusion that you have no choice,’ Samantha said. ‘I am so much happier to be my true self as a woman.
‘I always knew I was in the wrong body, even when I was really, really young, five or six-years-old.
‘But I grew up in Baghdad in the ’60s and the ’70s, so who would hear of anything about being transgender or having surgery?
‘So I buried it, and I thought I have to be conventional. I met a woman who I got on well with, and I got married and had children.’
Samantha says she feels that being a women is easier nowadays, compared to when she first transitioned back in the 1990s.
‘When I transitioned to a woman in 1997, things were really difficult for women generally,’ she said.  +8
+8
 +8
+8
Samantha (left in 2001) underwent her first gender reassignment surgery in 1997, in order to become Samantha for the first time. However, she decided to transition to a man in 2004 (right), as she thought it would help her re-connect with her children
‘Now, it’s not as bad for women. You get more equal opportunities at work. I haven’t noticed as much discrimination against women as there used to be.’
However, she explained how she has found the recent conversations around transgender women troubling.
‘Before my surgery it was quite difficult, because there was all this debate about what is the difference between transgender females and real females, and whether transgender women are accepted as real women,’ she explained.
‘But I felt I had no choice [but go ahead with the operation], because I knew it was what would make me happy and make me complete as a woman.
‘I had to go ahead with it at all costs, essentially.’  +8
+8
Samantha (pictured in 1998 following her first gender reassignment operation) explained how she became estranged from her two children after divorcing his wife Trudi, following his decision to transition to a woman
Following her gender reassignment surgery, Samantha says she has been getting a lot of interest in the romance department – although she wants to enjoy being single for now.
‘I want to enjoy being single for a while, and not to rush. Rushing into relationships is quite difficult for someone who doesn’t even have my history.
‘I’m probably one of a handful of people in the whole world who has had a sex transition three times.
‘You need someone with a pHD to understand what I’ve gone through,’ she explained.
‘But one should always be open to love. I could love a man, I could love a woman, as long as there feels like there’s a connection – that’s what I’m looking for.’
Samantha Kane’s new book Mohammed and Susan (Diversity Books, £8.99) is out on September 6.
Comment I first heard of Samantha Kane while in conversation with Dr Russell Reid in 2003 , the year I wrote ‘Man , Maid, Woman’. Reid was facing legal action from Ms Kane for wrongfull daignosis and rushing her case. Dr Reid , a ground breaking gender psychiatrist, earned a reputation for prescribing hormone drugs following just one consultation. This led to a flurry of complaints , an inquiry and Dr Reid being banned from sole practice. He was effectively retired from his West London practice because of it.
Meanwhile , the ultra wealthy Samanatha Kane – formerly Charles – had featured in a number of news articles and a TV documentary where she was shown on the bridge of her new luxury yacht and preparing for a second sex change back to male. Charles reborn , was shown driving his ex army Landrover through London’s West End and talking of his hopes to meet an ‘English Rose.’
In a subsequent news feature Charles Kane II spoke of life as a woman. He said he noticed how long it took ‘sis’ women to choose clothes in a dress shop , while Samantha knew exactly what she wanted. Charles also observed that Samantha was not taken as seriously in business , alluding to being patronised. One is tempted to comment that she made the right decision to go back to female because , like so many women she just couldn’t make up her mind.
As far as being patronised , Roberta Jane Cook certainly experienced that. She also knew what clothes to buy and wear . I suspect that might have something to do with age because modern young women are not subject to the same influences and role models. Everyday fashion is tacky , so choosing one piece of trash from another is a bit difficult.
As for not being allowed to see her children , that has to do with ‘sis’ women believing that ‘sis’ womanhood is a God given sacred state of being and innocence – the Vigin Mother Mary ideology. Hence , as well as threatened by the competition and loss of male scapegoats, they regard transsexual as unclean mad perverts. Facts.
Meanwhile , successful transsexuals like Stephanie Ann Lloyd and Jan Morris quietly did their own thing , comfortable as women and living a life outside the LGBTQI fortress that bigots require them to live in. This is a country still dominated by Christian and Islamic.Judaic hypocrisy. R.J Cook

R,J Cook.
Cogito ergo sum – Posted with comment by R.J Cook
It may seem odd to post an article on Descartean dualism on one of the two toxic transgender clinic pages. The ignorant usually think only of sex and kinky cross dressers when it comes to those who ‘think’ they are the opposite sex. Some feminists become incredibly hostile , seeing MTF as a threat to their self righteous hectoring hegemony.
Many men are attracted to male to certain female transsexuals because those ‘women’ aspire to an old fashioned caring and elegant image which is no longer commonplace as average women become ever more assertive , competitive, aggrieved and disgruntled.
However, the body clearly plays an important part in their ‘gender identity.’ The methods used to diagnose gender identity issues , as per the the likes of Britain’s Tavistock Gender Identity Clinic are vague , in my view , ideological and based on the general premise that those who choose it are not mentally ill.
However, they cover themselves against misconduct claims, with the interesting statement that , many of their patients have other mental health problems so bad that they might commit suicide – begging the question how can seriously mentally ill people be trusted when they pesent themselves as transgendered in the first place ? . On the basis of ‘inductive logic’ ( contrdictions in terms ) they argue that every case is successful dignosis because far more of their ‘successes’ would have killed themselves without the surgery.
Philosophy was one of my six compulsory foundation year subjects from an intensive economics and economic history degree course at the University of East Anglia in the early 1970s. I found the subject perplexing and seemingly hard to follow. Descartes was early on the agenda and seemed like nonsense.. I was even more perplexed when my philosophy tutor told me that my work and seminar contributions were outstanding and that I should choose it as my major subject.
I chose not to because it didn’t seem like a real subject. However , when I attended an old faculty meeting in 2005, I ended up giving it a forceful defence from attack by a thundering woman mourning the demise of sociology at the University.
By this time , life had taught me the great value of ‘truth’ seeking philosophy. As a former college lecturer and Oxford University A level examiner, I had formed the conclusion that so called Critical Sociology , along with Critical Race Theory , had no claim to truth seeking. It was pure ideology with a subtle social engineering agenda. The police love it. So, after my talk, Tim O’Hagan Professor Emeritus in philosophy, thanked me heartily while vigorously shaking my hand.
I must however, conclude that Descartes had good ideas but the mind would be rather lonely and poorly defined – like Krang from The Turtles’ – without a body. Having said that, I knew a man a few years ago who was run over aged 7 , most of his body paralysed for the next 70 years. That body could not function properly without his brain , and vice versa. There is evidence that memories and other data are stored in other organs and have been transferred to other people via transplants.
The beauty of honest philosophy is that its proponents keep on asking questions. The ugliness of modern sociology is in the way it is warped and fixed for oppresive control purposes in the modern Police State. It is all very well to offer the alleged freedoms of gender choice , but the thinking behind it is suspect. If the mind is separate then it shouldn’t matter what the body is. If the body and mind talk to each other , it poses the question which department makes the gender switch choice and why ? Or is the issue being resolved by the State’s social engineers to resolve some very serious problems and tensions that the ruling elite have deliberately caused ?
R.J Cook
Image Appledene Archives.
René Descartes:
The Mind-Body Distinction

One of the deepest and most lasting legacies of Descartes’ philosophy is his thesis that mind and body are really distinct—a thesis now called “mind-body dualism.” He reaches this conclusion by arguing that the nature of the mind (that is, a thinking, non-extended thing) is completely different from that of the body (that is, an extended, non-thinking thing), and therefore it is possible for one to exist without the other. This argument gives rise to the famous problem of mind-body causal interaction still debated today: how can the mind cause some of our bodily limbs to move (for example, raising one’s hand to ask a question), and how can the body’s sense organs cause sensations in the mind when their natures are completely different? This article examines these issues as well as Descartes’ own response to this problem through his brief remarks on how the mind is united with the body to form a human being. This will show how these issues arise because of a misconception about Descartes’ theory of mind-body union, and how the correct conception of their union avoids this version of the problem. The article begins with an examination of the term “real distinction” and of Descartes’ probable motivations for maintaining his dualist thesis.
Table of Contents
- What is a Real Distinction?
- Why a Real Distinction?
- The Real Distinction Argument
- The Mind-Body Problem
- Descartes’ Response to the Mind-Body Problem
- References and Further Reading
1. What is a Real Distinction?
It is important to note that for Descartes “real distinction” is a technical term denoting the distinction between two or more substances (see Principles, part I, section 60). A substance is something that does not require any other creature to exist—it can exist with only the help of God’s concurrence—whereas, a mode is a quality or affection of that substance (see Principles part I, section 5). Accordingly, a mode requires a substance to exist and not just the concurrence of God. Being sphere shaped is a mode of an extended substance. For example, a sphere requires an object extended in three dimensions in order to exist: an unextended sphere cannot be conceived without contradiction. But a substance can be understood to exist alone without requiring any other creature to exist. For example, a stone can exist all by itself. That is, its existence is not dependent upon the existence of minds or other bodies; and, a stone can exist without being any particular size or shape. This indicates for Descartes that God, if he chose, could create a world constituted by this stone all by itself, showing further that it is a substance “really distinct” from everything else except God. Hence, the thesis that mind and body are really distinct just means that each could exist all by itself without any other creature, including each other, if God chose to do it. However, this does not mean that these substances do exist separately. Whether or not they actually exist apart is another issue entirely.
2. Why a Real Distinction?
A question one might ask is: what’s the point of arguing that mind and body could each exist without the other? What’s the payoff for going through all the trouble and enduring all the problems to which it gives rise? For Descartes the payoff is twofold. The first is religious in nature in that it provides a rational basis for a hope in the soul’s immortality [because Descartes presumes that the mind and soul are more or less the same thing]. The second is more scientifically oriented, for the complete absence of mentality from the nature of physical things is central to making way for Descartes’ version of the new, mechanistic physics. This section investigates both of these motivating factors.
a. The Religious Motivation
In his Letter to the Sorbonne published at the beginning of his seminal work, Meditations on First Philosophy, Descartes states that his purpose in showing that the human mind or soul is really distinct from the body is to refute those “irreligious people” who only have faith in mathematics and will not believe in the soul’s immortality without a mathematical demonstration of it. Descartes goes on to explain how, because of this, these people will not pursue moral virtue without the prospect of an afterlife with rewards for virtue and punishments for vice. But, since all the arguments in the Meditations—including the real distinction arguments— are for Descartes absolutely certain on a par with geometrical demonstrations, he believes that these people will be obliged to accept them. Hence, irreligious people will be forced to believe in the prospect of an afterlife. However, recall that Descartes’ conclusion is only that the mind or soul can exist without the body. He stops short of demonstrating that the soul is actually immortal. Indeed, in the Synopsis to the Mediations, Descartes claims only to have shown that the decay of the body does not logically or metaphysically imply the destruction of the mind: further argumentation is required for the conclusion that the mind actually survives the body’s destruction. This would involve both “an account of the whole of physics” and an argument showing that God cannot annihilate the mind. Yet, even though the real distinction argument does not go this far, it does, according to Descartes, provide a sufficient foundation for religion, since the hope for an afterlife now has a rational basis and is no longer a mere article of faith.
b. The Scientific Motivation
The other motive for arguing that mind and body could each exist without the other is more scientifically oriented, stemming from Descartes’ intended replacement of final causal explanations in physics thought to be favored by late scholastic-Aristotelian philosophers with mechanistic explanations based on the model of geometry. Although the credit for setting the stage for this scholastic-Aristotelian philosophy dominant at Descartes’ time should go to Thomas Aquinas (because of his initial, thorough interpretation and appropriation of Aristotle’s philosophy), it is also important to bear in mind that other thinkers working within this Aristotelian framework such as Duns Scotus, William of Ockham, and Francisco Suarez, diverged from the Thomistic position on a variety of important issues. Indeed, by Descartes’ time, scholastic positions divergent from Thomism became so widespread and subtle in their differences that sorting them out was quite difficult. Notwithstanding this convoluted array of positions, Descartes understood one thesis to stand at the heart of the entire tradition: the doctrine that everything ultimately behaved for the sake of some end or goal. Though these “final causes,” as they were called, were not the only sorts of causes recognized by scholastic thinkers, it is sufficient for present purposes to recognize that Descartes believed scholastic natural philosophers used them as principles for physical explanations. For this reason, a brief look at how final causes were supposed to work is in order.
Descartes understood all scholastics to maintain that everything was thought to have a final cause that is the ultimate end or goal for the sake of which the rest of the organism was organized. This principle of organization became known as a thing’s “substantial form,” because it was this principle that explained why some hunk of matter was arranged in such and such a way so as to be some species of substance. For example, in the case of a bird, say, the swallow, the substantial form of swallowness was thought to organize matter for the sake of being a swallow species of substance. Accordingly, any dispositions a swallow might have, such as the disposition for making nests, would then also be explained by means of this ultimate goal of being a swallow; that is, swallows are disposed for making nests for the sake of being a swallow species of substance. This explanatory scheme was also thought to work for plants and inanimate natural objects.
A criticism of the traditional employment of substantial forms and their concomitant final causes in physics is found in the Sixth Replies where Descartes examines how the quality of gravity was used to explain a body’s downward motion:
But what makes it especially clear that my idea of gravity was taken largely from the idea I had of the mind is the fact that I thought that gravity carried bodies toward the centre of the earth as if it had some knowledge of the centre within itself (AT VII 442: CSM II 298).
On this pre-Newtonian account, a characteristic goal of all bodies was to reach its proper place, namely, the center of the earth. So, the answer to the question, “Why do stones fall downward?” would be, “Because they are striving to achieve their goal of reaching the center of the earth.” According to Descartes, this implies that the stone must have knowledge of this goal, know the means to attain it, and know where the center of the earth is located. But, how can a stone know anything? Surely only minds can have knowledge. Yet, since stones are inanimate bodies without minds, it follows that they cannot know anything at all—let alone anything about the center of the earth.
Descartes continues on to make the following point:
But later on I made the observations which led me to make a careful distinction between the idea of the mind and the ideas of body and corporeal motion; and I found that all those other ideas of . . . ‘substantial forms’ which I had previously held were ones which I had put together or constructed from those basic ideas (AT VII 442-3: CSM II 298).
Here, Descartes is claiming that the concept of a substantial form as part of the entirely physical world stems from a confusion of the ideas of mind and body. This confusion led people to mistakenly ascribe mental properties like knowledge to entirely non-mental things like stones, plants, and, yes, even non-human animals. The real distinction of mind and body can then also be used to alleviate this confusion and its resultant mistakes by showing that bodies exist and move as they do without mentality, and as such principles of mental causation such as goals, purposes (that is, final causes), and knowledge have no role to play in the explanation of physical phenomena. So the real distinction of mind and body also serves the more scientifically oriented end of eliminating any element of mentality from the idea of body. In this way, a clear understanding of the geometrical nature of bodies can be achieved and better explanations obtained.
3. The Real Distinction Argument
Descartes formulates this argument in many different ways, which has led many scholars to believe there are several different real distinction arguments. However, it is more accurate to consider these formulations as different versions of one and the same argument. The fundamental premise of each is identical: each has the fundamental premise that the natures of mind and body are completely different from one another.
The First Version
The first version is found in this excerpt from the Sixth Meditation:
[O]n the one hand I have a clear and distinct idea of myself, in so far as I am simply a thinking, non-extended thing [that is, a mind], and on the other hand I have a distinct idea of body, in so far as this is simply an extended, non-thinking thing. And accordingly, it is certain that I am really distinct from my body, and can exist without it (AT VII 78: CSM II 54).
Notice that the argument is given from the first person perspective (as are the entire Meditations). This “I” is, of course, Descartes insofar as he is a thinking thing or mind, and the argument is intended to work for any “I” or mind. So, for present purposes, it is safe to generalize the argument by replacing “I” with “mind” in the relevant places:
- I have a clear and distinct idea of the mind as a thinking, non-extended thing.
- I have a clear and distinct idea of body as an extended, non-thinking thing.
- Therefore, the mind is really distinct from the body and can exist without it.
At first glance it may seem that, without justification, Descartes is bluntly asserting that he conceives of mind and body as two completely different things, and that from his conception, he is inferring that he (or any mind) can exist without the body. But this is no blunt, unjustified assertion. Much more is at work here: most notably what is at work is his doctrine of clear and distinct ideas and their veridical guarantee. Indeed the truth of his intellectual perception of the natures of mind and body is supposed to be guaranteed by the fact that this perception is “clear and distinct.” Since the justification for these two premises rests squarely on the veridical guarantee of whatever is “clearly and distinctly” perceived, a brief side trip explaining this doctrine is in order.
Descartes explains what he means by a “clear and distinct idea” in his work Principles of Philosophy at part I, section 45. Here he likens a clear intellectual perception to a clear visual perception. So, just as someone might have a sharply focused visual perception of something, an idea is clear when it is in sharp intellectual focus. Moreover, an idea is distinct when, in addition to being clear, all other ideas not belonging to it are completely excluded from it. Hence, Descartes is claiming in both premises that his idea of the mind and his idea of the body exclude all other ideas that do not belong to them, including each other, and all that remains is what can be clearly understood of each. As a result, he clearly and distinctly understands the mind all by itself, separately from the body, and the body all by itself, separately from the mind.
According to Descartes, his ability to clearly and distinctly understand them separately from one another implies that each can exist alone without the other. This is because “[e]xistence is contained in the idea or concept of every single thing, since we cannot conceive of anything except as existing. Possible or contingent existence is contained in the concept of a limited thing…” (AT VII 166: CSM II 117). Descartes, then, clearly and distinctly perceives the mind as possibly existing all by itself, and the body as possibly existing all by itself. But couldn’t Descartes somehow be mistaken about his clear and distinct ideas? Given the existence of so many non-thinking bodies like stones, there is no question that bodies can exist without minds. So, even if he could be mistaken about what he clearly and distinctly understands, there is other evidence in support of premise 2. But can minds exist without bodies? Can thinking occur without a brain? If the answer to this question is “no,” the first premise would be false and, therefore, Descartes would be mistaken about one of his clear and distinct perceptions. Indeed, since we have no experience of minds actually existing without bodies as we do of bodies actually existing without minds, the argument will stand only if Descartes’ clear and distinct understanding of the mind’s nature somehow guarantees the truth of premise 1; but, at this point, it is not evident whether Descartes’ “clear and distinct” perception guarantees the truth of anything.
However, in the Fourth Meditation, Descartes goes to great lengthsto guarantee the truth of whatever is clearly and distinctly understood. This veridical guarantee is based on the theses that God exists and that he cannot be a deceiver. These arguments, though very interesting, are numerous and complex, and so they will not be discussed here. Suffice it to say that since Descartes believes he has established God’s inability to deceive with absolute, geometrical certainty, he would have to consider anything contradicting this conclusion to be false. Moreover, Descartes claims that he cannot help but believe clear and distinct ideas to be true. However, if God put a clear and distinct idea in him that was false, then he could not help but believe a falsehood to be true and, to make matters worse, he would never be able to discover the mistake. Since God would be the author of this false clear and distinct idea, he would be the source of the error and would, therefore, be a deceiver, which must be false. Hence, all clear and distinct ideas must be true, because it is impossible for them to be false given God’s non-deceiving nature.
That said, the clarity and distinctness of Descartes’ understanding of mind and body guarantees the truth of premise 1. Hence, both “clear and distinct” premises are not blunt, unjustified assertions of what he believes but have very strong rational support from within Descartes’ system. However, if it turns out that God does not exist or that he can be a deceiver, then all bets are off. There would then no longer be any veridical guarantee of what is clearly and distinctly understood and, as a result, the first premise could be false. Consequently, premise 1 would not bar the possibility of minds requiring brains to exist and, therefore, this premise would not be absolutely certain as Descartes supposed. In the end, the conclusion is established with absolute certainty only when considered from within Descartes’ own epistemological framework but loses its force if that framework turns out to be false or when evaluated from outside of it.
These guaranteed truths express some very important points about Descartes’ conception of mind and body. Notice that mind and body are defined as complete opposites. This means that the ideas of mind and body represent two natures that have absolutely nothing in common. And, it is this complete diversity that establishes the possibility of their independent existence. But, how can Descartes make a legitimate inference from his independent understanding of mind and body as completely different things to their independent existence? To answer this question, recall that every idea of limited or finite things contains the idea of possible or contingent existence, and so Descartes is conceiving mind and body as possibly existing all by themselves without any other creature. Since there is no doubt about this possibility for Descartes and given the fact that God is all powerful, it follows that God could bring into existence a mind without a body and vice versa just as Descartes clearly and distinctly understands them. Hence, the power of God makes Descartes’ perceived logical possibility of minds existing without bodies into a metaphysical possibility. As a result, minds without bodies and bodies without minds would require nothing besides God’s concurrence to exist and, therefore, they are two really distinct substances.
The Second Version
The argument just examined is formulated in a different way later in the Sixth Meditation:
[T]here is a great difference between the mind and the body, inasmuch as the body is by its very nature always divisible, while the mind is utterly indivisible. For when I consider the mind, or myself in so far as I am merely a thinking thing, I am unable to distinguish any parts within myself; I understand myself to be something quite single and complete….By contrast, there is no corporeal or extended thing that I can think of which in my thought I cannot easily divide into parts; and this very fact makes me understand that it is divisible. This one argument would be enough to show me that the mind is completely different from the body…. (AT VII 86-87: CSM II 59).
This argument can be reformulated as follows, replacing “mind” for “I” as in the first version:
- I understand the mind to be indivisible by its very nature.
- I understand body to be divisible by its very nature.
- Therefore, the mind is completely different from the body.
Notice the conclusion that mind and body are really distinct is not explicitly stated but can be inferred from 3. What is interesting about this formulation is how Descartes reaches his conclusion. He does not assert a clear and distinct understanding of these two natures as completely different but instead makes his point based on a particular property of each. However, this is not just any property but a property each has “by its very nature.” Something’s nature is just what it is to be that kind of thing, and so the term “nature” is here being used as synonymous with “essence.” On this account, extension constitutes the nature or essence of bodily kinds of things; while thinking constitutes the nature or essence of mental kinds of things. So, here Descartes is arguing that a property of what it is to be a body, or extended thing, is to be divisible, while a property of what it is to be a mind or thinking thing is to be indivisible.
Descartes’ line of reasoning in support of these claims about the respective natures of mind and body runs as follows. First, it is easy to see that bodies are divisible. Just take any body, say a pencil or a piece of paper, and break it or cut it in half. Now you have two bodies instead of one. Second, based on this line of reasoning, it is easy to see why Descartes believed his nature or mind to be indivisible: if a mind or an “I” could be divided, then two minds or “I’s” would result; but since this “I” just is my self, this would be the same as claiming that the division of my mind results in two selves, which is absurd. Therefore, the body is essentially divisible and the mind is essentially indivisible: but how does this lead to the conclusion that they are completely different?
Here it should be noted that a difference in just any non-essential property would have only shown that mind and body are not exactly the same. But this is a much weaker claim than Descartes’ conclusion that they are completely different. For two things could have the same nature, for example, extension, but have other, changeable properties or modes distinguishing them. Hence, these two things would be different in some respect, for example, in shape, but not completely different, since both would still be extended kinds of things. Consequently, Descartes needs their complete diversity to claim that he has completely independent conceptions of each and, in turn, that mind and body can exist independently of one another.
Descartes can reach this stronger conclusion because these essential properties are contradictories. On the one hand, Descartes argues that the mind is indivisible because he cannot perceive himself as having any parts. On the other hand, the body is divisible because he cannot think of a body except as having parts. Hence, if mind and body had the same nature, it would be a nature both with and without parts. Yet such a thing is unintelligible: how could something both be separable into parts and yet not separable into parts? The answer is that it can’t, and so mind and body cannot be one and the same but two completely different natures. Notice that, as with the first version, mind and body are here being defined as opposites. This implies that divisible body can be understood without indivisible mind and vice versa. Accordingly each can be understood as existing all by itself: they are two really distinct substances.
However, unlike the first version, Descartes does not invoke the doctrine of clear and distinct ideas to justify his premises. If he had, this version, like the first, would be absolutely certain from within Descartes’ own epistemological system. But if removed from this apparatus, it is possible that Descartes is mistaken about the indivisibility of the mind, because the possibility of the mind requiring a brain to exist would still be viable. This would mean that, since extension is part of the nature of mind, it would, being an extended thing, be composed of parts and, therefore, it would be divisible. As a result, Descartes could not legitimately reach the conclusion that mind and body are completely different. This would also mean that the further, implicit conclusion that mind and body are really distinct could not be reached either. In the end, the main difficulty with Descartes’ real distinction argument is that he has not adequately eliminated the possibility of minds being extended things like brains.
4. The Mind-Body Problem
The real distinction of mind and body based on their completely diverse natures is the root of the famous mind-body problem: how can these two substances with completely different natures causally interact so as to give rise to a human being capable of having voluntary bodily motions and sensations? Although several versions of this problem have arisen over the years, this section will be exclusively devoted to the version of it Descartes confronted as expressed by Pierre Gassendi, the author of the Fifth Objections, and Descartes’ correspondent, Princess Elizabeth of Bohemia. Their concern arises from the claim at the heart of the real distinction argument that mind and body are completely different or opposite things.
The complete diversity of their respective natures has serious consequences for the kinds of modes each can possess. For instance, in the Second Meditation, Descartes argues that he is nothing but a thinking thing or mind, that is, Descartes argues that he is a “thing that doubts, understands, affirms, denies, is willing, is unwilling, and also imagines and has sensory perceptions” (AT VII 28: CSM II 19). It makes no sense to ascribe such modes to entirely extended, non-thinking things like stones, and therefore, only minds can have these kinds of modes. Conversely, it makes no sense to ascribe modes of size, shape, quantity and motion to non-extended, thinking things. For example, the concept of an unextended shape is unintelligible. Therefore, a mind cannot be understood to be shaped or in motion, nor can a body understand or sense anything. Human beings, however, are supposed to be combinations of mind and body such that the mind’s choices can cause modes of motion in the body, and motions in certain bodily organs, such as the eye, cause modes of sensation in the mind.
The mind’s ability to cause motion in the body will be addressed first. Take for example a voluntary choice, or willing, to raise one’s hand in class to ask a question. The arm moving upward is the effect while the choice to raise it is the cause. But willing is a mode of the non-extended mind alone, whereas the arm’s motion is a mode of the extended body alone: how can the non-extended mind bring about this extended effect? It is this problem of voluntary bodily motion or the so-called problem of “mind to body causation” that so troubled Gassendi and Elizabeth. The crux of their concern was that in order for one thing to cause motion in another, they must come into contact with one another as, for example, in the game of pool the cue ball must be in motion and come into contact with the eight-ball in order for the latter to be set in motion. The problem is that, in the case of voluntarily bodily movements, contact between mind and body would be impossible given the mind’s non-extended nature. This is because contact must be between two surfaces, but surface is a mode of body, as stated at Principles of Philosophy part II, section 15. Accordingly, the mind does not have a surface that can come into contact with the body and cause it to move. So, it seems that if mind and body are completely different, there is no intelligible explanation of voluntary bodily movement.
Although Gassendi and Elizabeth limited themselves to the problem of voluntary bodily movement, a similar problem arises for sensations, or the so-called problem of “body to mind causation.” For instance, a visual sensation of a tree is a mode of the mind alone. The cause of this mode would be explained by the motion of various imperceptible bodies causing parts of the eye to move, then movements in the optic nerve, which in turn cause various “animal spirits” to move in the brain and finally result in the sensory idea of the tree in the mind. But how can the movement of the “animal spirits,” which were thought to be very fine bodies, bring about the existence of a sensory idea when the mind is incapable of receiving modes of motion given its non-extended nature? Again, since the mind is incapable of having motion and a surface, no intelligible explanation of sensations seems possible either. Therefore, the completely different natures of mind and body seem to render their causal interaction impossible.
The consequences of this problem are very serious for Descartes, because it undermines his claim to have a clear and distinct understanding of the mind without the body. For humans do have sensations and voluntarily move some of their bodily limbs and, if Gassendi and Elizabeth are correct, this requires a surface and contact. Since the mind must have a surface and a capacity for motion, the mind must also be extended and, therefore, mind and body are not completely different. This means the “clear and distinct” ideas of mind and body, as mutually exclusive natures, must be false in order for mind-body causal interaction to occur. Hence, Descartes has not adequately established that mind and body are two really distinct substances.
5. Descartes’ Response to the Mind-Body Problem
Despite the obviousness of this problem, and the amount of attention given to it, Descartes himself never took this issue very seriously. His response to Gassendi is a telling example:
These questions presuppose amongst other things an explanation of the union between the soul and the body, which I have not yet dealt with at all. But I will say, for your benefit at least, that the whole problem contained in such questions arises simply from a supposition that is false and cannot in any way be proved, namely that, if the soul and the body are two substances whose nature is different, this prevents them from being able to act on each other (AT VII 213: CSM II 275).
So, Descartes’ response to the mind-body problem is twofold. First, Descartes contends that a response to this question presupposes an explanation of the union between the mind (or soul) and the body. Second, Descartes claims that the question itself stems from the false presupposition that two substances with completely different natures cannot act on each other. Further examination of these two points will occur in reverse order.
Descartes’ principles of causation put forward in the Third Meditation lie at the heart of this second presupposition. The relevant portion of this discussion is when Descartes argues that the less real cannot cause something that is more real, because the less real does not have enough reality to bring about something more real than itself. This principle applies on the general level of substances and modes. On this account, an infinite substance, that is, God, is the most real thing because only he requires nothing else in order to exist; created, finite substances are next most real, because they require only God’s creative and conservative activity in order to exist; and finally, modes are the least real, because they require a created substance and an infinite substance in order to exist. So, on this principle, a mode cannot cause the existence of a substance since modes are less real than finite substances. Similarly, a created, finite substance cannot cause the existence of an infinite substance. But a finite substance can cause the existence of another finite substance or a mode (since modes are less real than substances). Hence, Descartes’ point could be that the completely diverse natures of mind and body do not violate this causal principle, since both are finite substances causing modes to exist in some other finite substance. This indicates further that the “activity” of the mind on the body does not require contact and motion, thereby suggesting that mind and body do not bear a mechanistic causal relation to each other. More will be said about this below.
The first presupposition concerns an explanation of how the mind is united with the body. Descartes’ remarks about this issue are scattered across both his published works and his private correspondence. These texts indicate that Descartes did not maintain that voluntary bodily movements and sensation arise because of the causal interaction of mind and body by contact and motion. Rather, he maintains a version of the form-matter theory of soul-body union endorsed by some of his scholastic-Aristotelian predecessors and contemporaries. Although a close analysis of the texts in question cannot be conducted here, a brief summary of how this theory works for Descartes can be provided.
Before providing this summary, however, it is important to disclaim that this scholastic-Aristotelian interpretation is a minority position amongst Descartes scholars. The traditional view maintains that Descartes’ human being is composed of two substances that causally interact in a mechanistic fashion. This traditional view led some of Descartes’ successors, such as Malebranche and Leibniz (who also believed in the real distinction of mind and body), to devise metaphysical systems wherein mind and body do not causally interact despite appearances to the contrary. Other philosophers considered the mind-body problem to be insurmountable, thereby denying their real distinction: they claim that everything is either extended (as is common nowadays) or mental (as George Berkeley argued in the 18th century). Indeed, this traditional, mechanistic interpretation of Descartes is so deeply ingrained in the minds of philosophers today, that most do not even bother to argue for it. However, a notable exception is Marleen Rozemond, who argues for the incompatibility of Descartes’ metaphysics with any scholastic-Aristotelian version of mind or soul-body union. Those interested in closely examining her arguments should consult her book Descartes’s Dualism. A book arguing in favor of the scholastic-Aristotelian interpretation is entitled Descartes and the Metaphysics of Human Nature; Chapter 5 specifically addresses Rozemond’s concerns.
Two major stumbling blocks Rozemond raises for the scholastic-Aristotelian interpretation concern the mind’s status as a substantial form and the extent to which Descartes can maintain a form of the human body. However, recall that Descartes rejects substantial forms because of their final causal component. Descartes’ argument was based on the fact (as he understood it) that the scholastics were ascribing mental properties to entirely non-mental things like stones. Since the mind is an entirely mental thing, these arguments just do not apply to it. Hence, Descartes’ particular rejection of substantial forms does not necessarily imply that Descartes did not view the mind as a substantial form. Indeed, as Paul Hoffman noted:
Descartes really rejects the attempt to use the human soul as a model for explanations in the entirely physical world. This makes it possible that Descartes considered the human mind to be the only substantial form. At first glance this may seem ad hoc but it is also important to notice that rejecting the existence of substantial forms with the exception of the mind or rational soul was not uncommon amongst Descartes’ contemporaries.
Although the mind’s status as a substantial form may seem at risk because of its meager explicit textual support, Descartes suggests that the mind a “substantial form” twice in a draft of open letter to his enemy Voetius:
Yet, if the soul is recognized as merely a substantial form, while other such forms consist in the configuration and motion of parts, this very privileged status it has compared with other forms shows that its nature is quite different from theirs (AT III 503: CSMK 207-208).
Descartes then remarks “this is confirmed by the example of the soul, which is the true substantial form of man” (AT III 508: CSMK 208). Although other passages do not make this claim explicitly, they do imply (in some sense) that the mind is a substantial form. For instance, Descartes claims in a letter to Mesland dated 9 February 1645, that the soul is “substantially united” with the human body (AT IV 166: CSMK 243). This “substantial union” was a technical term amongst the scholastics denoting the union between a substantial form and matter to form a complete substance. Consequently, there is some reason for believing that the human mind is the only substantial form left standing in Descartes’ metaphysics.
Another major stumbling block recognized by Rozemond is the extent to which, if any, Descartes’ metaphysics can maintain a principle for organizing extension into a human body. This was a point of some controversy amongst the scholastics themselves. Philosophers maintaining a Thomistic position argued that the human soul is the human body’s principle of organization. While others, maintaining a basically Scotistic position, argued that some other form besides the human soul is the form of the body. This “form of corporeity” organizes matter for the sake of being a human body but does not result in a full-fledged human being. Rather it makes a body with the potential for union with the human soul. The soul then actualizes this potential resulting in a complete human being. If Descartes did hold a fundamentally scholastic theory of mind-body union, then is it more Thomistic or Scotistic? Since intellect and will are the only faculties of the mind, it does not have the faculty for organizing matter for being a human body. So, if Descartes’ theory is scholastic, it must be most in line with some version of the Scotistic theory. Rozemond argues that Descartes’ rejection of all other substantial forms (except the human mind or soul) precludes this kind of theory since he cannot appeal to the doctrine of substantial forms like the Scotists.
Although Descartes argues that bodies, in the general sense, are constituted by extension, he also maintains that species of bodies are determined by the configuration and motion of their parts. This doctrine of “configuration and motion of parts” serves the same purpose as the doctrine of substantial forms with regards to entirely physical things. But the main difference between the two is that Descartes’ doctrine does not employ final causes. Recall that substantial forms organize matter for the purpose of being a species of thing. The purpose of a human body endowed with only the form of corporeity is union with the soul. Hence, the organization of matter into a human body is an effect that is explained by the final cause or purpose of being disposed for union. But, on Descartes’ account, the explanatory order would be reversed: a human body’s disposition for union is an effect resulting from the configuration and motion of parts. So, even though Descartes does not have recourse to substantial forms, he still has recourse to the configuration of matter and to the dispositions to which it gives rise, including “all the dispositions required to preserve that union” (AT IV 166: CSMK 243). Hence, on this account, Descartes gets what he needs, namely, Descartes gets a body properly configured for potential union with the mind, but without recourse to the scholastic notion of substantial forms with their final causal component.
Another feature of this basically Scotistic position is that the soul and the body were considered incomplete substances themselves, while their union results in one, complete substance. Surely Descartes maintains that mind and body are two substances but in what sense, if any, can they be considered incomplete? Descartes answers this question in the Fourth Replies. He argues that a substance may be complete insofar as it is a substance but incomplete insofar as it is referred to some other substance together with which it forms yet some third substance. This can be applied to mind and body as follows: the mind insofar as it is a thinking thing is a complete substance, while the body insofar as it is an extended thing is a complete substance, but each taken individually is only an incomplete human being.
This account is repeated in the following excerpt from a letter to Regius dated December 1641:
For there you said that the body and the soul, in relation to the whole human being, are incomplete substances; and it follows from their being incomplete that what they constitute is a being through itself (that is, an ens per se; AT III 460: CSMK 200).
The technical sense of the term “being through itself” was intended to capture the fact that human beings do not require any other creature but only God’s concurrence to exist. Accordingly, a being through itself, or ens per se, is a substance. Also notice that the claim in the letter to Regius that two incomplete substances together constitute a being through itself is reminiscent of Descartes’ remarks in the Fourth Replies. This affinity between the two texts indicates that the union of mind and body results in one complete substance or being through itself. This just means that mind and body are the metaphysical parts (mind and body are incomplete substances in this respect) that constitute one, whole human being, which is a complete substance in its own right. Hence, a human being is not the result of two substances causally interacting by means of contact and motion, as Gassendi and Elizabeth supposed, but rather they bear a relation of act and potency that results in one, whole and complete substantial human being.
This sheds some light on why Descartes thought that an account of mind-body union would put Gassendi’s and Elizabeth’s concerns to rest: they misconceived the union of mind and body as a mechanical relation when in fact it is a relation of act and potency. This avoids Gassendi’s and Elizabeth’s version of this problem. This aversion is accomplished by the fact that modes of voluntary motion (and sensations, by extrapolation) should be ascribed to a whole human being and not to the mind or the body taken individually. This is made apparent in a 21 May 1643 letter to Elizabeth where Descartes distinguishes between various “primitive notions.” The most general are the notions of being, number, duration, and so on, which apply to all conceivable things. He then goes on to distinguish the notions of mind and body:
Then, as regards body in particular, we have only the notion of extension, which entails the notions of shape and motion; and as regards the soul on its own, we have only the notion of thought, which includes the perceptions of the intellect and the inclinations of the will (AT III 665: CSMK 218).
Here body and soul (or mind) are primitive notions and the notions of their respective modes are the notions “entailed by” or “included in” these primitives. Descartes then discusses the primitive notion of mind-body union:
Lastly, as regards the soul and the body together, we have only the notion of their union, on which depends our notion of the soul’s power to move the body, and the body’s power to act on the soul and cause its sensations and passions (AT III 665: CSMK 218).
In light of the immediately preceding lines, this indicates that voluntary bodily movements and sensations are not modes of the body alone, or the mind alone, but rather are modes of “the soul and the body together.” This is at least partially confirmed in the following lines from Principles, part I, article 48:
But we also experience within ourselves certain other things, which must not be referred either to the mind alone or to the body alone. These arises, as will be made clear in the appropriate place, from the close and intimate union of our mind with the body. This list includes, first, appetites like hunger and thirds; secondly, the emotions or passions . . . (AT VIIIA 23: CSM I 209).
These texts indicate that the mind or soul is united with the body so as to give rise to another whole complete substance composed of these two metaphysical parts. And, moreover, this composite substance now has the capacity for having modes of its own, namely, modes of voluntary bodily movement and sensation, which neither the mind nor the body can have individually. So, voluntary bodily movements are not modes of the body alone caused by the mind, nor are sensations modes of the mind alone caused by the body. Rather, both are modes of a whole and complete human being. On this account, it makes no sense to ask how the non-extended mind can come into contact with the body to cause these modes. To ask this would be to get off on the wrong foot entirely, since contact between these two completely diverse substances is not required for these modes to exist. Rather all that is necessary is for the mind to actualize the potential in a properly disposed human body to form one, whole, human being to whom is attributed modes of voluntary movement and sensation.
Although the scholastic-Aristotelian interpretation avoids the traditional causal interaction problem based on the requirements of contact and motion, it does run up against another version of that problem, namely, a problem of formal causation. This is a problem facing any scholastic-Aristotelian theory of mind or soul-body union where the soul is understood to be an immaterial substantial form. Recall that the immaterial mind or soul assubstantial form is suppose to act on a properly disposed human body in order to result in a full-fledged human being. The problem of formal causal interaction is: how can an immaterial soul assubstantial form act on the potential in a material thing? Can any sense be made of the claim that a non-extended or immaterial things acts on anything? Descartes noticed in a letter to Regius (AT III 493: CSMK 206) that the scholastics did not try to answer this question and so he and Regius need not either. The likely explanation of their silence is that the act-potency relation was considered absolutely fundamental to scholastic-Aristotelian philosophy and, therefore, it required no further explanation. So, in the end, even if Descartes’ theory is as described here, it does not evade all the causal problems associated with uniting immaterial souls or mind to their respective bodies. , However, if this proposed account is true, it helps to cast Descartes’ philosophy in a new light and to redirect the attention of scholars to the formal causal problems involved.
6. References and Further Reading
Primary Sources
- Descartes, Rene, Ouevres de Descartes, 11 vols., eds. Charles Adam and Paul Tannery, Paris: Vrin, 1974-1989.
- This is still the standard edition of all of Descartes’ works and correspondence in their original languages. Cited in the text as AT, volume, page.
- Descartes, Rene, The Philosophical Writings of Descartes, 3 vols., trans. John Cottingham, Robert Stoothoff, Dugald Murdoch and Anthony Kenny, Cambridge: Cambridge University Press, 1984-1991
- This is the standard English translation of Descartes philosophical works and correspondence. Cited in the text as CSM or CSMK, volume, page.
Secondary Sources
- Broughton, Janet and Mattern, Ruth, “Reinterpreting Descartes on the Notion of the Union of Mind and Body,” Journal of the History of Philosophy 16 (1978), 23-32.
- A reinterpretation of the notion of mind-body union in the correspondence with Elizabeth, which addresses Radner’s interpretation of it. See below.
- Garber, Daniel, “Understanding Interaction: What Descartes Should Have Told Elizabeth,” Southern Journal of Philosophy, Supp. 21 (1983), 15-32.
- Article addressing the issues of the primitive notions and how this theory should be used to explain mind-body causal interaction to Elizabeth.
- Hoffman, Paul, “The Unity of Descartes’ Man,” The Philosophical Review 95 (1986), 339-369.
- Article arguing that Descartes’ theory of mind-body union is more in line with scholastic-Aristotelian theories of soul-body union than previously supposed.
- Kenny, Anthony, Descartes: A Study of His Philosophy, New York: Random House, 1968. See especially chapters 4 and 10.
- These chapters provide classic interpretations of the real distinction between mind and body and the mind-body problem.
- Mattern, Ruth, “Descartes’ Correspondence with Elizabeth Concerning both the Union and Distinction of Mind and Body” in Descartes: Critical and Interpretive Essays, ed. Michael Hooker, Baltimore: John Hopkins University Press, 1978, 212-222.
- Short essay examining Descartes’ correspondence with Elizabeth on this issue and how it was supposed to direct her to a correct understanding of mind-body causal interaction.
- Radner, Daisie, “Descartes’ Notion of the Union of Mind and Body,” Journal of the History of Philosophy 9 (1971), 159-170.
- This is the first article in Anglo-American scholarship to address the issue of mind-body union. It addresses several texts, including the letter to Elizabeth enumerating the primitive notions.
- Rozemond, Marleen, Descartes’s Dualism, Cambridge: Harvard University Press, 1998.
- This book argues for a particular understanding of the real distinction between mind and body that would preclude Hoffman’s scholastic-Aristotelian account of their union.
- Skirry, Justin, Descartes and the Metaphysics of Human Nature, London and New York: Thoemmes-Continuum Press, 2005.
- This book takes issue with Rozemond’s account of the mind-body union through a close re-examination of fundamental features of Descartes’ metaphysics and by building on certain features of Hoffman’s account.
- Voss, Stephen, “Descartes: The End of Anthropology” in Reason, Will and Sensation, ed. John Cottingham, Oxford: Clarendon Press, 1994.
- This essay provides a close textual analysis of Descartes’ account of the union of mind and body on the supposition that he maintained a Platonic rather than scholastic-Aristotelian theory of mind-body union.
- Williams, Bernard, Descartes: The Project of Pure Enquiry, Sussex: Harvester Press, 1978. See especially chapter 4.
- This is another classic account of the mind-body relation in Descartes.
- Wilson, Margaret, Descartes, London and Boston: Routledge and Kegan Paul, 1978.
- Provides classic accounts of the real distinction argument and issues concerning mind-body causal interaction.
Author Information
vJustin Skirry
Email: jskirry@yahoo.com
U. S. A.
Why do so many teenage girls want to change gender? Posted April 5th 2021
In the last 10 years, there has been an extraordinary increase in teenagers seeking to transition from female to male. What’s behind it—and has the NHS been too quick to find a solution?
By Emma Hartley
It is commonly acknowledged that while biological sex is genetically determined, gender is a social construct. A human being cannot—and should not—be reduced to their biology, or indeed their genitals, because psychologically we are as much a product of the way that other people treat us as we are of our genetic inheritance. Homo sapiens are social creatures: our ability to cooperate is what gave us the evolutionary upper hand over our stronger Neanderthal cousins. Without parents, siblings, peers, colleagues, friends and lovers our idea of ourselves would remain ill-defined—we wouldn’t know who we were.
Imagine you were raised by wolves in a cave—let’s call you Mowgli—but then later met another human of the opposite sex. You would notice the physiological differences. But as to interpreting those differences, where would you start? Without being exposed to the concept of “man” or “woman”—let alone “laddish” or “girly”—you’d lack any mental map to provide the pointers to the typically “male” and “female” behaviour instilled in us by human society.
Precisely because gender is a social construct, the evolution of its boundaries and meanings will tell us something fundamental about our society. And gender-wise something really big is going on in the UK—but it’s not the big something you might think.
Transsexuality is a talking point like never before, and a glance at the figures sheds some light on why. The number of children, in particular, being referred to the Tavistock and Portman Foundation Trust’s gender identity development service (Gids)—the NHS service through which all UK candidates for a sex change under 18 are funnelled—is up from 77 in 2009 to 2,590 in 2018-9. But what’s almost as dramatic as the headline numbers are developments in who is transitioning. In November 2017, the Guardian reported that 70 per cent of referrals were female. This was a surprising statistic because only 10 years previously the overall ratio had been more like 75 per cent males seeking to be female, and indeed it is still the gender traffic in that direction that dominates the increasingly noisy, divisive and panic-inflected debate.
Recently, though, alarm bells have begun to ring among a handful of psychiatric professionals about the number of teenage girls arriving at the Tavistock’s door and the nature of their treatment. Right now a legal case is being brought by Susan Evans, a former psychiatric nurse at the Tavistock and Portman NHS Foundation Trust, alongside a parent of an autistic female child wishing to transition to be male, arguing that children are not legally capable of consenting to a gender transition. November last year saw the launch of the Detransition Advocacy Network, a UK group numbering several hundred members. And in January, the NHS announced an independent review into puberty suppressants and cross-sex hormone treatments, to be chaired by Hilary Cass, formerly president of the Royal College of Paediatrics and Child Health.
But until the end of 2019, you could be forgiven for thinking that a panic about trans women using the “wrong” toilet cubicles was the biggest gender issue of the day (instead of something that could be easily solved by affording everyone the same privacy). Whenever the issue flares up politically—as when the Labour leadership candidates were asked to sign a pledge that labelled trans rights sceptics as “hate groups,” or the Scottish government proposed reforms to allow a change of legal gender without a medical diagnosis of gender dysphoria—it always seems to come back to loos and changing rooms. These vitriolic debates keep bubbling up—especially online.
But there is a much bigger scandal brewing than any Twitterstorm. While there have been a great many thoughtful doctors at the Tavistock, the picture is sometimes disturbing. Marcus Evans, a psychotherapist and former governor of the Tavistock and Portman NHS Foundation Trust, resigned in February 2019, citing an institutional rush to prescribe puberty-blocking hormone treatment to children questioning their gender and who may wish to transition. “The Tavistock is behaving recklessly with these kids who are in a distressed state,” he claims. What’s especially odd about the alleged rush to prescribe rather than consider alternatives, he argues, is that this clinic’s international reputation was built on the quality of its talking therapy.
“Over the last five to 10 years there has been a complete change in the profile of the people presenting,” says Evans. “These children believe that they are in the wrong body and they are very persistent and forceful in saying that they want a solution—and that that is physical intervention. But I’ve been in psychiatry for 40 years and when people are in a distressed state they often narrow things down and fix on one thing as a solution, putting pressure on clinicians for a magic bullet.”
In psychiatry “generally,” he says, the aim is to “open things out,” and take the time to ask questions about “what is going on.” After all, “adolescence is a moving picture. We move through experimenting with different identities as our bodies change and our role in society changes. An individual has to tolerate a -certain amount of confusion and anxiety and we should be able to help with that through therapy.” But when it comes to “the Tavistock’s gender identity service,” he says, “this work has not been done… the entire area has become unnecessarily politicised.”
It is undeniable that trans people have faced discrimination and abuse from those who don’t understand their experiences. A vocal rights lobby is quick to push back against transphobia—both real and perceived. Sometimes, though, legitimate challenges tip over into intimidation.
An American academic, Lisa Littman, encountered strenuous opposition when she published an article that coined the term “rapid onset gender dysphoria.” She lost a consultancy job, though remained an assistant professor at Brown University School of Public Health. Littman identified knots of socially-awkward girls drawn together in online chat rooms who reinforced each other’s self-diagnosis of being transgender before presenting to medical professionals. She had been led there by research involving the parents of some of these children, who had mentioned that their offspring had friends who also identified as transgender. (The US is experiencing a similar shift towards female transitioners, as are Finland, Canada and the Netherlands among others.) Along with Marcus Evans, Littman has pointed to a high incidence of autism and eating disorders among the same patients who present as trans. That observation raises some obvious questions about the narrowness of an approach that fixates on hormonal treatment for gender dysphoria.
The Tavistock pushes back against accusations that it is too quick to assume its patients are transgender and to provide hormones. “Our work with young people is not to affirm or deny,” they told me. “We respect children and young people’s sense of themselves and our assessment process considers gender identity development within the context of a psychological, biological, developmental and social framework, meaning that it is designed to give assessors a broad picture of the young person’s past and current gender identification.” Their work, they went on, is “cautious” and “considered” and whatever clinical interventions they do undertake are “laid out in nationally-set service specifications.” Hormone blockers are prescribed. But surgery cannot be performed until the age of 18.
Anna Hutchinson, who worked at the Tavistock until 2017 as a clinical psychologist and who is now in private practice, isn’t convinced. She believes there is an uncritical “affirmation” of gender dysphoria and the Tavistock is not as “cautious” as it should be. “The young people are making sense of themselves in the best way they can,” she tells me. “They often aren’t aware of anything other than the affirmative approach for managing gender dysphoria.” If they heard “different points of view,” they might be better placed to make “balanced and informed decisions about what they need,” she suggests. She describes a rush to treat: “Affirmation involves a quick assessment and then you get them into the medical system, on to hormone blockers if this is age appropriate. The next step is cross-sex hormones with their irreversible effects. Nearly 100 per cent make that journey once they start on the blockers.”
Hutchinson suggested that I look at an advisory organisation called the World Professional Association for Transgender Health (WPATH), alleging that its “best-practice” guidelines in this field, which have been adhered to internationally and spread through professional development courses for practitioners, have often been activist-led rather than evidence-led. Critics charge that senior members of WPATH have been behaving as advocates for transsexuality, rather than dispassionate advisers on mental health. Indeed, such advocacy is included in WPATH’s mission statement.
The WPATH guidelines say that “children as young as two may show features that could indicate gender dysphoria. They may… prefer clothes, toys and games that are commonly associated with the other sex and may prefer playing with other-sex peers.” A very distinct perspective is on show here: one that venerates individual feelings of identity, and yet also regards the social categories of gender with such solemnity that a girl toddler’s fondness for toy tractors is now seen as a marker of dysphoria. There is little room for interrogating either the feelings or the categories: it’s the biology that needs to change.
The guidelines add: “Treatment aimed at trying to change a person’s gender identity and expression to become more congruent with sex assigned at birth has been attempted in the past without success… Such treatment is no longer considered ethical.” While the WPATH guidelines counsel against pathologising gender dysphoria, these guidelines arguably have the effect of pathologising the natal sex of the person in question.
WPATH has the level of influence that it does, it has been suggested to me, because until the sudden increase in numbers of people questioning their gender no one paid much attention. WPATH began as the Harry Benjamin International Gender Dysphoria Association in 1979, when there might only have been a few hundred patients a year presenting in the UK and these tended to be adult males. Each could be dealt with on a case-by-case basis. Given the vast and rapid increase in the number of people wanting to change gender, there is bound to be a danger that discretion goes out of the window, and “guidelines” become rigid rules. (WPATH did not respond to questions.)
“The WPATH guidelines may have had the effect of de-skilling professionals who have been trained to provide therapy,” says Hutchinson, adding that in Gids the clinic simply “can’t” provide the traditional therapy for which the Tavistock is known, and which medics from across the country might expect when they refer patients here.
Hutchinson points to Gids’s own service specification (which doesn’t include talking therapy as a long-term treatment option) and a memorandum about conversion therapy published by the UK Council for Psychotherapy in 2017. Along with the influence of WPATH it is, I think, the missing piece of the jigsaw that reveals how the “affirmation” approach to gender reassignment has become the norm in the UK.
“Different issues may have been conflated, despite the best of intentions,” explains Hutchinson. She argues that a “false equivalence” has been drawn between pro-active conversion therapy for sexuality, where clinicians attempt to alter patients’ sexual responses, and talking people into becoming more comfortable with their bodies. Non-medical therapy for people with gender dysphoria has come to be seen as effectively trying to argue them out of identifying as transgender, as people were once convinced that they shouldn’t be gay. But the distinction between medical acts and medical omissions has been lost somewhere here, a serious matter in a profession whose traditional starting point has been “First, do no harm.” (The Tavistock responds: “We operate with no preconceptions and outcomes for any given young person.”)
Traditional ideas about the physician assessing the patient in the round also seem at risk of being forgotten. “We generally don’t talk about the relevance of the incredibly high incidence of autism spectrum disorder among these new, young, female patients,” says Hutchinson. “Autism often also means black-and-white thinking and struggling with the onset of puberty, so we have to ask the question ‘can this simply be a coincidence?’” And can it be a coincidence, either, that the stampede to transition is so concentrated among girls and young women?
An instructive parallel case can be found in Eastern Europe. In the former Soviet bloc, and especially in 1980s Poland, more women than men requested sex changes. “Polish sexologists knew about this difference [with the west] and were startled by it,” said Ludmila Janion of Warsaw University, who recently completed a PhD on the subject.
Why was this? The experts I spoke to while researching a book in the 2000s suggested that the reverse statistics might have something to do with it being especially awful to be a female under Communism, propelling some to jump immediately from questioning their sexuality—“I’m not sure I’m straight”—to the conclusion: “I must be a man.”
Current figures are hard to come by in capitalist Poland, but a 3:1 ratio of women becoming men as against men becoming women has been suggested to me. So perhaps it was actually less about Communism, than more ingrained cultural issues. Anna Kłonkowska, a Polish academic living in New York, suggests interrogating the very words that Eastern Europeans use: “Slavic languages are highly gendered,” she explained. “There is no distinction possible within them between sex and gender: no separate words for these things. It is linguistically assumed that your anatomical features are the same as your perceived gender. It is not only the case with verbs (as in French) but also nouns and adjectives, and when you speak you express your gender in every sentence as well as the gender of the person to whom you are speaking.” Additionally, said Kłonkowska, “Cultural elevation of masculinity is built into the language: -transitioning female to male is seen as socially elevating whereas transitioning male to female is degrading.”
All of this makes conversation uncomfortable to anyone who is not quite sure where they fit in. Female to male trans people have told Kłonkowska that “their biggest concern” is “not really about the bodily alterations” but “merely being treated as male.” Unfortunately, in Poland, there is no way to have the one without the other. “Judges generally want to see some physical changes before they will allow the legal one. People say that they feel forced to take hormones so that a judge will see a man or a woman even though they are not unhappy with their existing bodies. Then afterwards they would give up taking the hormones.”
Whether the root cause is language, the legacy of Communism or patriarchal oppression, this is a story that needs to be understood at the level of society, not just the individual psyche. There is little doubt—as Janion argues—that there was traditionally “no cultural space for butch (ie more masculine) lesbians.” Transsexuality was perceived by the sexologists as a rare and difficult—but curable—illness. In this case it might have constituted a relatively attractive identity. After all, it turned a lesbian living with another woman into a success. Sexologists saw it as restoring “normal” heterosexuality. A similar trend can be seen in Iran, where gender reassignment surgery is encouraged for gay men who would otherwise be viciously persecuted.
“Whether someone will identify as trans or will be diagnosed as trans,” Janion argues, “will depend on what the other viable options are.” At which point it seems worth asking what, given the similar trend emerging in the UK and other western societies, might have changed to make so many youngsters born female feel so alienated in their own bodies?
A video of the launch of the recently constituted Detransition Advocacy Network sheds especially interesting light here on some young women’s struggles. The panel comprised of five women between 20 and 23 years old, plus the organiser, Charlie Evans, 28. All six are lesbians whose youthful feelings of self-loathing, self-disgust and social dislocation led them to make a decision to transition to male that they later came to regret, after varying degrees of hormone and surgical treatment.
Evans, in common with her panel-mates, now locates the source of her gender dysphoria as social (rather than personal)—and in particular in misogyny towards “masculine” women and lesbians. All six participants are now on better terms with their own lesbianism. “Gender dysphoria is the opposite of body positivity,” one of them says. But it was a harrowing and physically disruptive journey to have taken at such a young age. (All began their transition during puberty some time ago, and therefore have not been a part of the current controversy surrounding puberty-blocker drugs.) One man in the audience, audibly distressed at what he was hearing, asks: “How is it possible that you have had no one in your lives to tell you that it was OK just to be yourselves?”
There are broader questions here for UK society in 2020, and about its attitude to girls. It is hard not to feel that social media and porn have recently been conspiring to create a rigid and ultra “femme” idea of what a beautiful woman should look like. Whereas once Jamie Lee Curtis, with her short hair and athletic build, was considered a sex symbol in Hollywood, these days the Kardashians’ femininity can feel almost as homogenised as it is commoditised. And its shallow markers—nails, lashes, bling—frequently blur the distinction between the world’s most desirable women and drag queens. Keeping up with the requirements of womanhood, as they are understood in these times, imposes a time-sapping burden, and all those (most of us) who are not prepared to devote a large portion of our day to our appearance end up feeling alienated. Detransitioners might well be merely exposing the tip of an iceberg of social-media generated misery.
Phoebe Jones (not her real name) is a lesbian attracted to masculine women who mourns the shrinking of her dating pool. “I’ve always tended towards dating masculine-of-centre women,” she tells me, “I’ve never seen these women as having less of a claim on womanhood than I do… Their self-acceptance was important to me as it allowed me to celebrate them.”
The trappings of femininity can be oppressive.
But it’s not always easy. One lesbian friend was raped by a classmate when she came out. Another “was cripplingly insecure in clothes but confident naked. I gently pointed out to her that her body wasn’t the problem. She breast-bound and tentatively used gender neutral pronouns. We became good friends. Now she sees herself as a woman and a lesbian and still looks like a boy. I get the feeling she is comfortable being desired as such these days, and desiring too.”
This success story speaks of a relatively “masculine” woman learning to find her psychological comfort publicly and privately—something far too rarely reflected in the media in the era of Love Island. Such happy negotiations of identity remain largely unacknowledged—to the detriment of others who are still stuck with the anguish that preceded the happy resolution.
“Increasingly on dating apps,” explains Jones, “masculine lesbians use they/them pronouns… If anything, it almost seems more common now than just being a proudly butch lesbian, particularly in younger women.”
Jones is at pains to point out that she does not have a problem with people transitioning, “if they are old enough and have had appropriate therapeutic support. But when it comes to adolescent girls wanting to transition, I find it very sad… I had terrible mental health as a teenager and if the same kind of agonising and reckless drive towards destruction and away from discomfort is shared by any of these girls, I can’t help but mourn the trend to assist them in taking this drive to the logical extreme rather than helping them learn to live with themselves. I mean, to help them learn to cope with their internal contradictions for at least long enough that a decision to transition is an adult, reflective and thoughtful decision.”
Many outside and indeed within the UK’s Gids service fear that, far from freeing people from the constraints of “being in the wrong body,” over the last 10 years the Tavistock has—with the best of intentions—been giving effect to some of society’s unkindest (if internalised) prejudices. What a tragedy it would be, if in trying to learn from the historic misstep of gay conversion therapy, we are allowing a rushed regime of transitioning young people that will one day be remembered in an equally controversial way. History does not repeat itself, but it does rhyme.
We want to hear what you think about this article. Submit a letter to letters@prospect-magazine.co.uk
© 2021 Prospect Publishing Limited

The following post will only make sense if read in conjunction with posts on About R.J Cook. The missing dynamic here is the police, which the NHS bodies refuse to admit or explain. This is the draft of a letter circulated to a number of lawyers for the purpose of staying within Statute of Limitations as all relevant public bodies refuse to explain anything, other than to label me as paranoid, ultimately bound for death by misadventure, hospitalisation, suicide or jail.
Ramsay, the psychiatrist ( sic ) noted in his report that if I saw all of the official records held on me, then I would be ‘upset.’ Fancy telling that to a person you have diagnosed as paranoid !The following was addressed to a specific lawyer. Obviously when they inquired they were told that I am subject to an ongoing police investigation and dangerous. R.J Cook December 4th 2020
“‘Thanks for getting back to me and I apologise for the delay in replying. I have given an outline of my situation below, as briefly as possible. More details and documents are available, if you feel you can help and proceed. My health is getting worse as a result of all that has happened to me. I thank you for your kind attention.
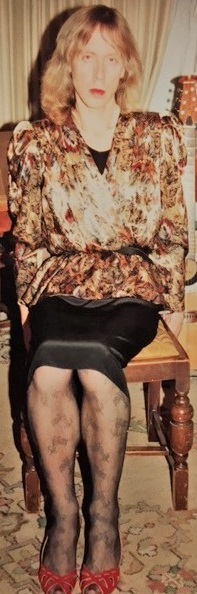

Image Appledene Photographics.

Image Appledene Photographics.
Man, Maid, Woman: Amazon.co.uk: Cook, Rj: 9781904408048 …
www.amazon.co.uk › Man-Maid-Woman-Rj-Cook
Buy Man, Maid, Woman by Cook, Rj (ISBN: 9781904408048) from Amazon’s Book Store. Everyday low prices and free delivery on eligible orders.
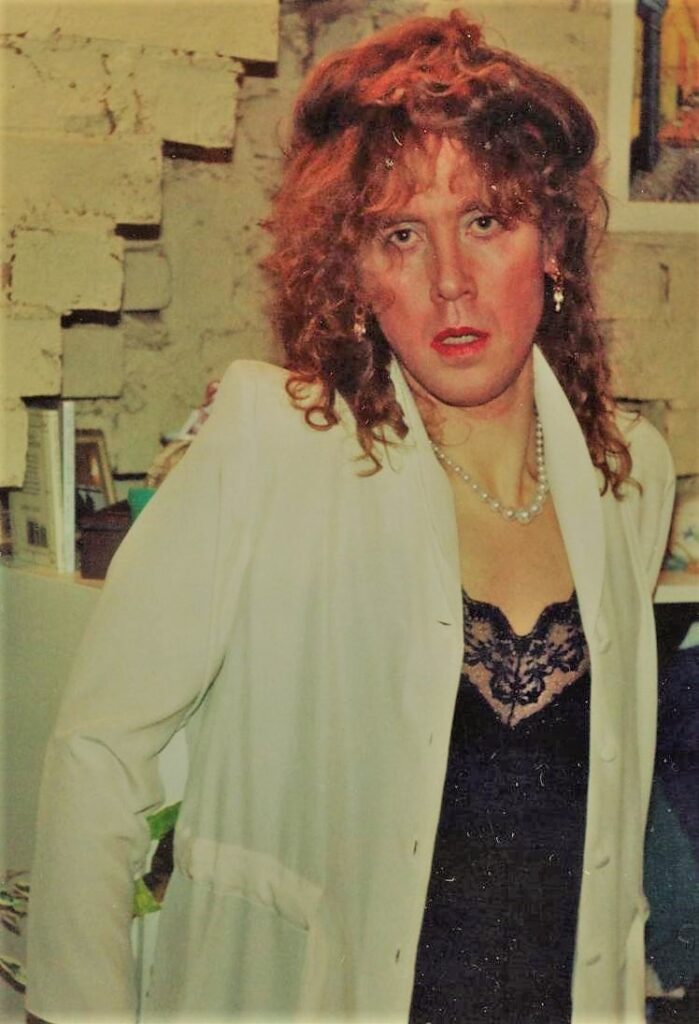
Summary of case involving Roberta Jane Cook
In 2016, I made an appointment at my local surgery with Dr Baines Clark, of Norden House Surgery, reference the possibility of me being transgendered. That surgery is Norden House Avenue Road Winslow, Bucks MK18. She referred me to Dr C.R Ramsay, a consultant pyschiatrist at Aylesbury’s Whiteleaf Centre. specialising in geriatric mental health care. He confrmed that I was in good physical and mental health – I have his report from 2016 confirming that I am suffering from no known mental illness . Ramsay concluded that I was a suitable candidate for the GIC and their services.
I then attended the GIC Clinic, had various assessments and consultations, but when it came to medication there were.several communications made known to me where Dr Roger Dickson of Norden House raised questions about my mental health and told them that my alleged heavy drinking meant my liver would struggle with hormone treatment. I was copied in to Dickson’s correspondence by Leighton Seal of the GIC who thanked Dickson for ‘five interesting letters.’
Dickson’s surgery had also ignored my prostate concerns since 2003 and my seriously raised free testosterone and abnormal Sex Hormone Binding Globulin ( SHBG ) levels on the basis that this was probabaly linked to alcohol abuse. By the way, I am not a heavy drinker and spent years working as an HGV driver until lockdown.).’This correspondence, from Dickson to Leighton Sea,l came one year after I had changed my name and conformed to their dress and behaviour requirements. I was offered no explanation or evidence.
As a matter of fact, taking anti androgens and alcohol is a serious health risk, so if I was a ‘drinker’ they were negligent at the GIC or suspected Dickson of lying. I am hypothyroid so regular liver and kidney function blood checks were routine for me. Dickson and his colleagues had regfularly signed me off on medicals as fit to drive HGVs, noting that I was not an alcoholic or mentally ill.
Dr Leighton Seal of the GIC overruled Norden House. Hormones, anti androgens and injections effectively chemically castrating me were prescribed. By February 2018, I was overdue to be listed for GRS ( Gender Reassignment Surgery ).
So, at my February 2018 meeting with Dr Kirpal Sahota of the GIC , Dr Sahota announced, apparently out of the blue, that my GRS was conditional on me taking anti psychotic drugs. She also said that I needed sessions with a psychiatrist from the Whiteleaf Centre. She had a male colleague present with a view to my long term therapy under this dangerous medication. Had the GIC et al done their job properly, and this not being connected with Norden House misconduct, then this medication with reasons would have been mentioned to me at the beginning – not after high risk hormone and anti androgen treatment. As it was, hormones, anti androgens, injections, facial hair removal and conforming to their dress code, my identity had been overwhelmed and myself put at risk from hate crime and social ostracism. In this context, I was suddenly expected to take anti psychotics, function and survive.
The situation is now compounded by Covid 19 lockdown, my son and I facing homelessness because of what has been done to me. One does not have to be mad to commit suicide – they know that. My ex wife admitted her habit of hitting me, and there was much worse, leading me to attempt hanging from a door handle in March 2007. You need to know this as my medical records appear to be subject to edit and direction. My ex wife was a senior employee of Dr Roger Dickson & Co – my GP practice. I also spent several years working there as a handyman, attending their social functions. My work there included extending the staff car park using a large digger, plumbing and re roofing an outbuilding.
As a psychology post grad, I had knowledge of anti psychotics, how they work, purpose and side effects. I was simply told that they would make me better without being told why they suddenly thought I was seriously mentally ill. Offering a path to over due GRS, Dr Sahota’s words were. ‘We would like you to take the medication, it will make you feel better and then we can deal with the GRS. Is that a deal ?’ I said no, also refusing the group therapy sessions and Whiteleaf psychiatric consultations. By this time my body was physically altered, along with hormone effects on my mental state. My genitals have since wasted away to the point where GRS would be very difficult if at all possible to any good worth while effect. Still Norden House, Whiteleaf and the GIC refuse to explain anything relating to me and gender reassignement..
The same month in 2018, prior to Ramsay’s visits., Sahota wrote to my GP, copying me in to a letter she had sent to my GP, informing him that I had secure female identity and was keen to proceed fo GRS. The letter approved further castration injections with the purpose of reducing my testosterone level to the approved level for surgery. Curiously, a few days later, psychiatrist, Dr C.R Ramsay arrived unannouced, along with a medical student and mental health nurse. I had just returned from a 13 hour HGV – which Ramsay turned into alcoholism, along with calling my efforts to defend myself ‘pressured speech’ which was a sign of a paranoid personality disorder – his ultimate and damning diagnosis..
I was warned that hospital was a possibility, so would best invite them in if I wanted a chance to avoid that. Two further afternnon sessions followed, both times after I had been at work – my usual work start times were between 0100 and 0200 hours. This is relevant because it was my custom to sip a glass of wine after work and prior to bed before my next shift
I protested against Ramsay’s intrusions.
After my third consultation, and well over a month later Ramsay phoned to ask me if I would accept a second opinion because GIC ‘wanted something stronger’ than he had written about me. I was working at the time, but he persisted. I told him that it was up to him to make that decision. I later discovered that Ramsay had already informed the GIC that I had refused a second opinion before he even asked me. Ramsay concluded that I have abnormal psychology as well as paranoia and recommended a multi agency approach to monitoring me, but ‘hospital is not needed yet;’ He also concluded that I am anti social, secretive and cannot relate to others or sustain relationships. That was 2 years ago.
Neither Norden House. Whiteleaf or GIC have so far responded to the questions raised here. Obviously I have thought of suicide in this impossible situation. Paranoia is ‘abnormal suspicion’, schizophrenia is normally taken as multiple personality. I have had no empirically based explanation as to why they suggest all of this applies to me, and if it does then why were these agencies so careless and incompetent as to not notice before February 2018 and when GRS should have been imminent. If they had this view before then, why not act and why not eplain themselves to myself or my son ?
Several months ago Dr Kimble, of Norden House, wrote informing me that he had written to ask the GIC for an update on my status with them. I wrote thanking him, noting it would be interesting as to their reply, regarding what they did or didn’t say. Not surprsingly, I have not been told anything. .
So, in conclusion, if there is any truth in allegations and mental health diagnoses , then the key question is why on earth was I ever recommended for such serious gender re assignment treatment, lasting for 2 years, what were the reasons, the details of diagnosis etc ?. If they do not stick by their allegations and diagnosis, why not because it obviously implicates them in misconduct and misdiagnosis otherwise ? They were asking me at the GIC to take take very dangerous anti psychotics. as part of a bargain for sex change surgery ? That is serious, demanding serious explanation, the details should be provided on paper, also explaining all parties involved and why it took so long. They have refused to do that by ignoring all of my requests.
So the situation pertains and worsens. The effect on my physical and mental health has been extreme, my alarm and distress is ongoing – worsening in fact. The physical and psychologcal damage is dreadful and on going. leaving me in gender limbo, impotent and infertile. There is clear evidence of prejudice, malpractice, medical neglect, questionable diagnosis and practice – with external influence and malice that needs to be verified and explained to me in writing..I can answer any questions arising from what the various involved parties may offer in their defence. All concerned have had ample opportunity to explain themselves to me. I think their silence says a lot about them.
Yours Sincerely R.J Cook “
‘I make no judgement about gender brains , but it should be obvious that hormones and childhood are additiona factors , not just which type of sperm fertilises the egg. No one can really define or understand consciousnes and our sense of I. Emotions separate us from robots.
So my emotions told me that Maragaret Thatcher was an arrogant know all from a horrible little obscure place called Grantham. This prototype liberated female said many things including the line ” I went to Oxford University , but I didn’t let it hold me back.”
This is an extract from the song I was singing about her when this photo was taken :
‘There’ll alwys be an England as long as there is me
‘There’ll always be a golf course and Dennis on the tee
‘Oh we have sold the gas works, the telephonses as well
‘And we are busy thinking of other things to sell
‘My plans they know no limit
‘I, going on and on
‘And England as you knew it will pretty soon be gone. ‘ R.J Cook 1988
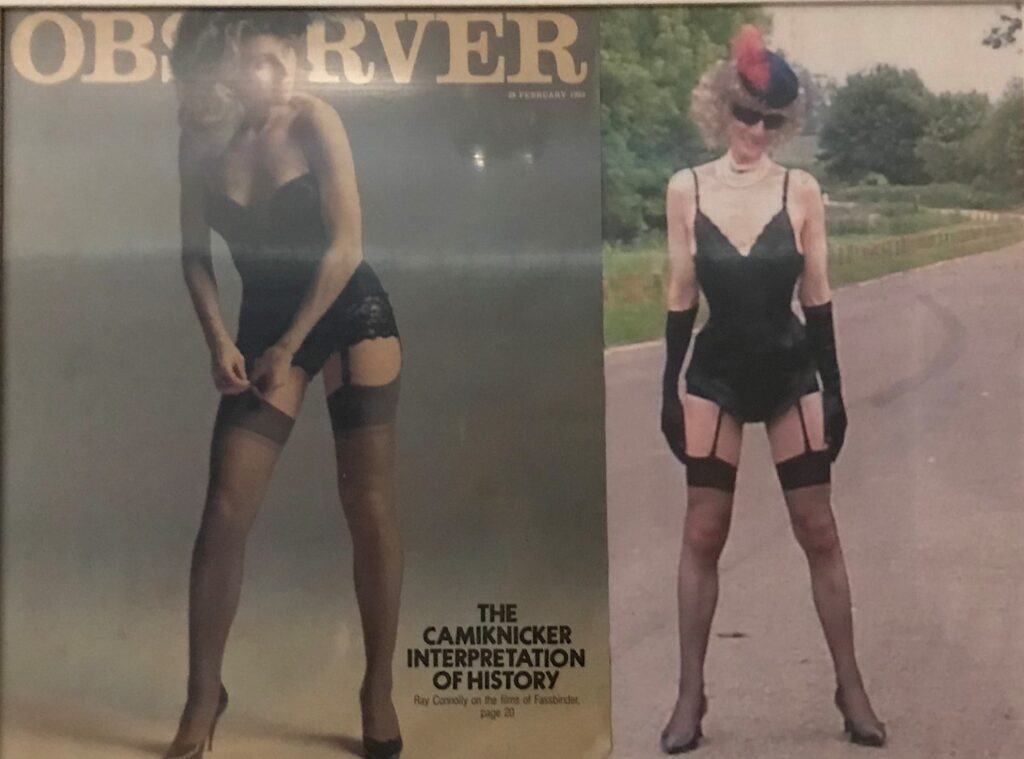
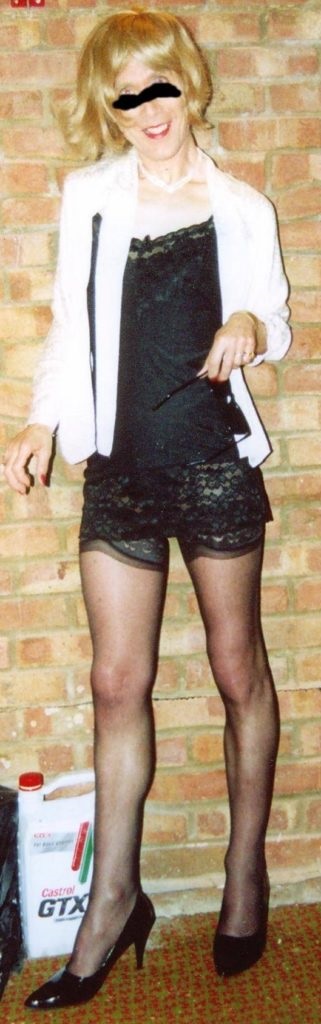
Their mental health has declined accordingly. They blame ‘privileged white men’ when they should be looking at themselves. They lie about abuse and rape , lay down endless rules and then wonder why men need viagra , effectively a date rape drug.
They make continuous demands for ever more internet controls and hate laws to protect themselves from criticism because they really believe in their own superiority. How deluded , how danggerous because they are running the show outside of the equally probelmatic Islamic world. R.J Cook.
Image Appledene Photographics.
